-
PDF
- Split View
-
Views
-
Cite
Cite
Eoghan P Burke, Patricia Harkins, Ilona Arih, Gerry O’Donoghue, A case of ectopic liver tissue adherent to the gallbladder, Journal of Surgical Case Reports, Volume 2018, Issue 6, June 2018, rjy128, https://doi.org/10.1093/jscr/rjy128
Close - Share Icon Share
Abstract
We report a case of a 30-year-old lady who presented to the emergency department with a 1 day history of severe epigastric pain which radiated to the back. Focused history, physical exam findings, haematological and radiological investigations, including ultrasound scanning of the abdomen, supported the diagnosis of acute gallstone pancreatitis. She was managed conservatively and underwent elective laparoscopic cholecystectomy at a later date. Intraoperatively, there was noted to be a small nodule loosely adherent to the gallbladder serosa. Histology from this nodule revealed it to be a portion of anatomically normal liver parenchyma also referred to as ectopic liver tissue (ELT). ELT is a rare developmental abnormality in which normally functioning liver tissue develops at an extra-hepatic site. ELT is known to have an increased risk of neoplastic transformation and so we believe it to be of clinical importance.
INTRODUCTION
Ectopic liver tissue (ELT) is a rare developmental abnormality in which normally functioning liver tissue develops at an extra-hepatic site and has no connection to the true liver. This is in contrast to the accessory lobe of the liver which has an anatomical connection to the liver proper. ELT has been reported in multiple intra-abdominal and thoracic sites including the kidneys, heart and pleural cavity [1–3]. The incidence of ELT is debated and widely felt to be underestimated. ELT rarely presents symptomatically and is often diagnosed at autopsy or following surgery for another reason [4]. However, because of the increased risk of hepatocellular carcinoma associated with ELT, we believe it to be an important congenital abnormality.
CASE REPORT
Ms X, a previously well 30-year-old lady, presented herself to the emergency department complaining of a 1 day history of severe epigastric pain. It came on suddenly overnight and woke her from sleep. It radiated through to her back. At its worst, she graded it as 10/10. This pain was associated with nausea and two episodes of vomiting. She denied any change in bowel habit, any dark urine or pale stool. Similarly, she denied any urinary symptoms and her last menstrual period was 3 weeks previously. She denied any recent alcohol intake.
On physical examination, she was mildly tender in the epigastrium and right hypochondium. There was no guarding or rigidity and bowel sounds were present. Vitals were all within normal limits on review in the ED.
Bloods (see Fig. 1) were notable for an elevated amylase, gamma GT and alanaine aminotransferase. C-reactive protein was also elevated. Chest X-ray was normal and did not indicate any free air under the diaphragm. Ultrasound of the abdomen was performed and identified a gallbladder containing multiple small gallstones. There was no evidence of gallbladder wall thickening or intra/extra-hepatic bile duct dilatation (Fig. 2).
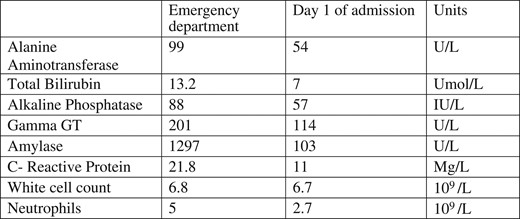
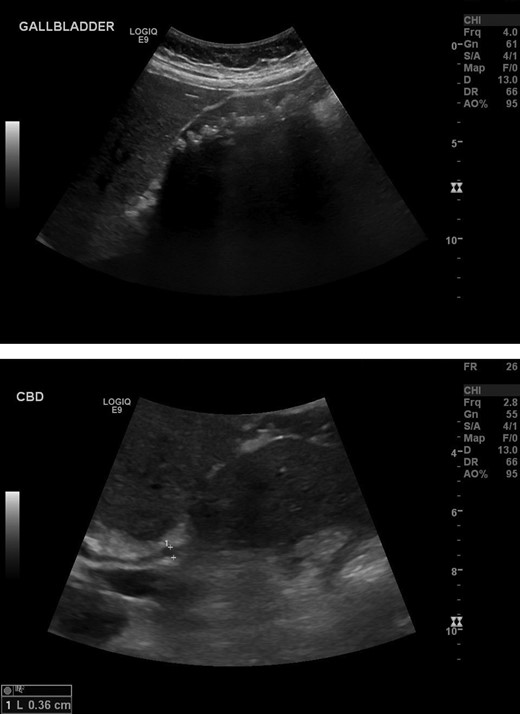
Extensive number of shadowing gallstones in the gallbladder. Negative for thickening of the anterior gallbladder wall. Negative for intra or extra-hepatic biliary dilatation.
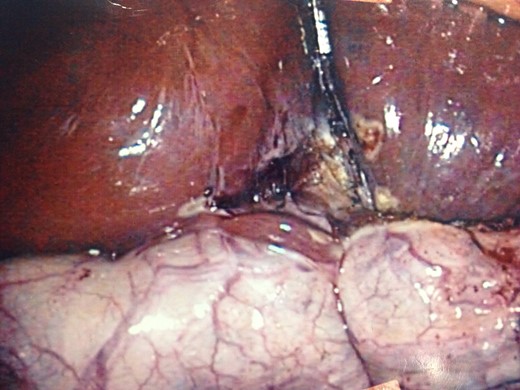
Intraoperative photo displaying gallbladder reflected superiorly, liver inferiorly and small nodule of normal liver parenchyma adherent to the gallbladder.
In light of these findings, Ms X was admitted as an Imrie 0 pancreatitis for observation over night. The following day she had clinically improved with resolution of the abdominal pain and tenderness. Bloods had also improved with a fall in amylase and CRP (see Fig. 1).
Ms X was discharged and brought back 1 month later for elective laparoscopic cholecystectomy. She tolerated the procedure well with no immediate complications. Intraoperatively, there was noted to be a small nodule loosely adherent to the gallbladder serosa (Fig. 3). This nodule was removed en-bloc with the gallbladder.
Histology identified this nodule to be a portion of normal liver parenchyma without any connection to the Liver proper, i.e ELT
DISCUSSION
ELT is a rare developmental abnormality in which liver tissue develops at an extra-hepatic site with no communication with the liver proper [4]. The true incidence is unknown as it is widely felt to be under-reported. A large study which reviewed over 5500 autopsy cases identified only 13 cases of ELT, another large study which reviewed 1802 laparoscopic cholecystectomy cases identified 12 cases of ELT [5, 6].
The precise mechanism behind the development of ELT is poorly understood. The most common site for ELT is the gallbladder although it has been found at various sites including the pancreas, adrenal glands, spleen, falciform ligament, pylorus, retroperitoneally, as well as in the thoracic cavity. An overarching theory has yet to explain its development in such diverse locations [7].
ELT is usually asymptomatic and generally found intraoperatively during surgeries performed for another reason, or at autopsy. However ELT is subject to the same pathologies as the liver proper and on occasion has been reported to cause symptoms, predominantly chronic abdominal pain, secondary to torsion or haemorrhage [4].
Importantly ELT does not contain a complete physiological hepatic lobule architecture often lacking a complete vascular and ductal system. This in turn often leads to the ELT being exposed to carcinogenic material for a prolonged duration which facilitates the carcinogenic process. This is thought to account for the significant observation that ELT seems predisposed to neoplastic transformation independent of the liver proper [8].
ELT is a rare entity. Due to its predominantly asymptomatic nature, it is rarely diagnosed pre-operatively. However due to its documented increased risk of neoplastic transformation, it seems prudent to remove the ELT when identified serendipitously intraoperatively. Increased awareness of this congenital anomaly may result in increased detection rates among radiologists in the future.
CONFLICT OF INTEREST STATEMENT
None declared.



