-
PDF
- Split View
-
Views
-
Cite
Cite
A E Fanshawe, H E C Hamilton, J Constantinou, External iliac vein aneurysm: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2018, Issue 5, May 2018, rjy115, https://doi.org/10.1093/jscr/rjy115
Close - Share Icon Share
Abstract
Iliac vein aneurysms are extremely rare, even amongst vein aneurysms. We discuss the case of a 26-year-old man with an external iliac vein aneurysm, likely secondary to iatrogenic vascular trauma in the neonatal period. It is the first reported case of an iliac vein aneurysm presenting with lower urinary tract symptoms. Attempts at endovenous management were unsuccessful and therefore the patient underwent open aneurysmectomy. A PubMed literature search revealed a total of nine case reports of iliac vein aneurysms published in English since 2011. We discuss the aetiology, presentation, investigation and management of iliac vein aneurysms and compare to our own case.
INTRODUCTION
Iliac vein aneurysms are extremely rare, even amongst vein aneurysms. We discuss the case of an external iliac vein (EIV) aneurysm, likely secondary to iatrogenic vascular trauma in the neonatal period.
CASE REPORT
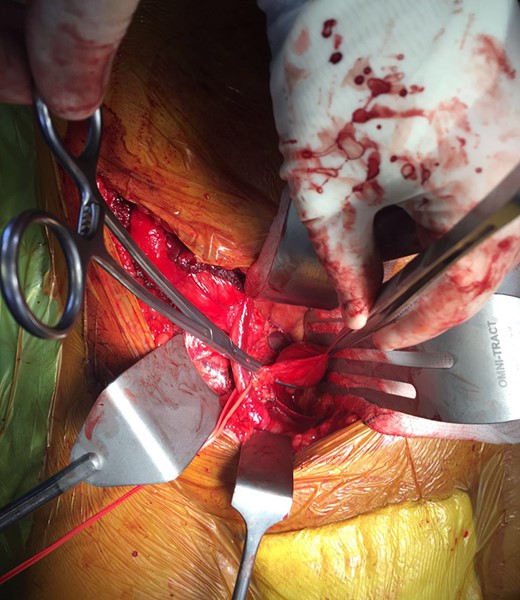
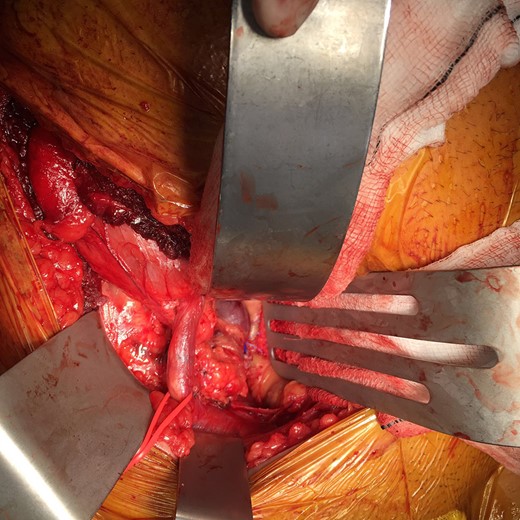
A 26-year-old man was referred to our vascular surgery tertiary referral service from his local hospital with leg size discrepancy (right > left) and prominent right leg varicose veins distally. He had lower urinary tract symptoms (frequency >30 times per day) for a year prior to presentation but had no leg symptoms in relation to his varicosities. His past medical history was of premature birth, as one of triplets, who spent a prolonged period on a neonatal intensive care unit. The patient thought he may have had a deep vein thrombosis in his right leg as a child. An MRI of his right thigh and pelvis demonstrated a 5 cm venous aneurysm (EIV), indenting the bladder, and generalized distal venous dilatation of both deep and superficial veins. He subsequently underwent venography, which confirmed an aneurysmal EIV, with massive collateral dilatation of trans-pelvic veins and complete occlusion of the right common femoral vein (CFV). A concurrent attempt at endovenous stenting was made, but was unsuccessful as the CFV could not be passed with a guide-wire and no alternate route was found possible. Further characterization by CT demonstrated a dilated and tortuous right internal iliac vein (IIV) feeding the aneurysm (Fig. 1). A multidisciplinary decision was made to proceed to operative repair, in light of the patient’s debilitating urinary frequency from the mass effect of the aneurysm. Pre-intervention venous severity scoring was not pursued as the patient’s symptoms were only bladder-related. The patient underwent an open aneurysmectomy via a Rutherford-Morrison incision, with concurrent right retrograde ureteric stent placement. Intra-operatively, a wide-necked aneurysm was confirmed to arise from the EIV (Fig. 2) in a saccular fashion. The aneurysm was clamped at the neck and closed with 3-0 Prolene (Ethicon, Inc., New Jersey, USA) leaving a normal calibre EIV (Figs 3 and 4). The IIV remained patent at the end of the procedure and a venous bypass was not performed. The patient recovered well post-operatively and was discharged home four days later, with removal of the ureteric stent prior to discharge. He has been followed up 6-monthly since and remains well at 2 years’ post-operatively. CT venogram has shown a good post-operative result, with no residual aneurysm (Fig. 5). The patient’s pre-operative lower urinary tract symptoms have improved. He did not develop any leg symptoms.
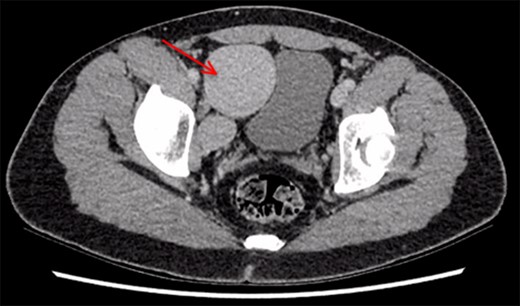
CT scan demonstrating right iliac vein aneurysm (5.7 cm) (red arrow) compressing the patient’s full bladder.
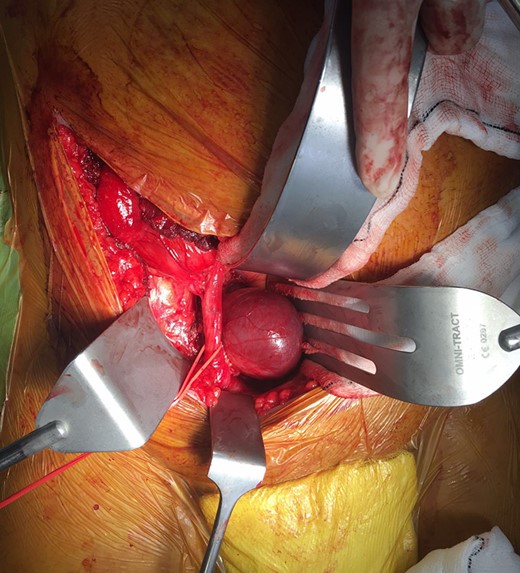
Intra-operative appearance of the external iliac vein aneurysm. A retroperitoneal approach was used via a Rutherford-Morrison incision. Laterally, the external iliac artery is controlled with a vessel loop.

Post-operative CT scan demonstrating no evidence of residual aneurysm, or bladder compression. A residual dilated and tortuous collateral vessel remains communicating between the right internal iliac vein and right common femoral vein (red arrow).
DISCUSSION
Vein aneurysms may be defined as solitary venous dilatations that communicate with a main venous structure, without contemporaneous arteriovenous fistulae [1]. Iliac vein aneurysms are extremely rare, even amongst vein aneurysms. Approximately 40 iliac territory venous aneurysms have been described in the existing literature. Zou et al. [2] performed a review of these up to 2011. We present a review of nine new cases in the literature that have been published since 2011 (Table 1). A systematic PubMed search was performed to identify these, using the search terms: iliac; vein; venous; aneurysm; external; internal in various combinations. All relevant articles written in English were reviewed.
The demographics, presentation, nature, location, size, imaging, management and outcome of iliac vein aneurysms reported in English since 2011 (PubMed search)
| Author . | Age and gender . | Symptoms . | Associated anomalies . | Primary or secondary? . | Location . | Size . | Imaging . | Management . | Outcome . |
|---|---|---|---|---|---|---|---|---|---|
| Fanshawe et al. 2017 (Current case) | 26M | Lower-urinary tract symptoms | DVT as a child | Secondary | Right EIV | 4 cm | CT, MRI and venography | Open aneurysmectomy with primary closure | Well, at 24 months post-op. CT confirming no residual aneurysm. Resolving lower urinary tract symptoms. |
| Audu et al. [1] | 63M | Left testicle and groin pain | Lower extremity varicose veins | Primary | Left IIV | 3.1 × 2.2 cm2 | MRI and venography | Endovenous embolisation | Symptom resolution at 1-month follow-up, with CT confirming aneurysmal occlusion. |
| Park et al. [4] | 63F | Acute severe abdominal pain | None | Primary | Right EIV | 4×5 cm2 | CT | Open aneurysmectomy with primary closure | Well, at months post-op, with Duplex USS every 6 months. |
| Shah et al. [8] | 22F | Incidental (found during work-up of bilateral acute limb ischaemia—treated with bilateral femoral embolectomies) | Patent foramen ovale; IVC obstruction; bilateral proximal common iliac stenoses | Primary | Right EIV | Not stated | CT | Open aneurysmorrhaphy with primary closure | Asymptomatic at 4-year follow-up, with surveillance Duplex USS demonstrating no recurrence. |
| Banzic et al. [9] | 24F | Non-healing skin ulceration below left knee | Misdiagnosis of Klippel–Trenaunay syndrome as a child; Right leg lengthening | Primary | Left CIV | 4 cm | CT, prior Duplex USS | Endovenous option presented; patient declined treatment. | Diagnosis of Parkes-Weber syndome (multiple AV fistulas throughout the left limb); Well at 2 years post diagnosis. |
| Escobar et al. [10] | 54F | Incidental (found during laparoscopic retroperitoneal dissection for endometrial adenocarcinoma) | None | Not stated | Right EIV | Not stated | Not performed | Not stated | Not stated. |
| Hosaka et al. [5] | 22F | Sudden-onset dyspnoea (PE) | None | Primary | Right EIV | 3.7 cm | CT | Open aneurysmectomy with great saphenous venous patch graft | Well, with patent EIV at 8-month follow-up. |
| Todorov et al. [6] | 62M | Incidental (elevated PSA) | Persistent left leg swelling following ankle fracture; Post-traumatic superficial femoral AV fistula of same leg (ligated years previously) | Secondary | Left EIV | 8 × 5×6 cm3 | CT, MRI and fluoroscopic venogram and IVUS intra-operatively | Endovenous stent graft | Stent graft patent, no leak and no migration. Resolution of left leg swelling. Annual follow-up with Duplex. |
| Javaraj et al. [7] | 37F | Left gluteal pain | None | Primary | Left EIV | 3.6 cm | Duplex USS, CT and venography | Hybrid repair with open aneurysmectomy and primary closure over angioplasty balloon as a mandrel | Post-op venography showing no residual aneurysm. Well, at 4 months post-op. |
| Zou et al. [2] | 14F | Sudden-onset dyspnoea and syncope (PE) | None | Primary | Left EIV | Not stated | Duplex USS, CT | Mechanical fragmentation and low-molecular weight anticoagulant for PE. Surgery offered; family declined further treatment. | Asymptomatic at 16 months. |
| Author . | Age and gender . | Symptoms . | Associated anomalies . | Primary or secondary? . | Location . | Size . | Imaging . | Management . | Outcome . |
|---|---|---|---|---|---|---|---|---|---|
| Fanshawe et al. 2017 (Current case) | 26M | Lower-urinary tract symptoms | DVT as a child | Secondary | Right EIV | 4 cm | CT, MRI and venography | Open aneurysmectomy with primary closure | Well, at 24 months post-op. CT confirming no residual aneurysm. Resolving lower urinary tract symptoms. |
| Audu et al. [1] | 63M | Left testicle and groin pain | Lower extremity varicose veins | Primary | Left IIV | 3.1 × 2.2 cm2 | MRI and venography | Endovenous embolisation | Symptom resolution at 1-month follow-up, with CT confirming aneurysmal occlusion. |
| Park et al. [4] | 63F | Acute severe abdominal pain | None | Primary | Right EIV | 4×5 cm2 | CT | Open aneurysmectomy with primary closure | Well, at months post-op, with Duplex USS every 6 months. |
| Shah et al. [8] | 22F | Incidental (found during work-up of bilateral acute limb ischaemia—treated with bilateral femoral embolectomies) | Patent foramen ovale; IVC obstruction; bilateral proximal common iliac stenoses | Primary | Right EIV | Not stated | CT | Open aneurysmorrhaphy with primary closure | Asymptomatic at 4-year follow-up, with surveillance Duplex USS demonstrating no recurrence. |
| Banzic et al. [9] | 24F | Non-healing skin ulceration below left knee | Misdiagnosis of Klippel–Trenaunay syndrome as a child; Right leg lengthening | Primary | Left CIV | 4 cm | CT, prior Duplex USS | Endovenous option presented; patient declined treatment. | Diagnosis of Parkes-Weber syndome (multiple AV fistulas throughout the left limb); Well at 2 years post diagnosis. |
| Escobar et al. [10] | 54F | Incidental (found during laparoscopic retroperitoneal dissection for endometrial adenocarcinoma) | None | Not stated | Right EIV | Not stated | Not performed | Not stated | Not stated. |
| Hosaka et al. [5] | 22F | Sudden-onset dyspnoea (PE) | None | Primary | Right EIV | 3.7 cm | CT | Open aneurysmectomy with great saphenous venous patch graft | Well, with patent EIV at 8-month follow-up. |
| Todorov et al. [6] | 62M | Incidental (elevated PSA) | Persistent left leg swelling following ankle fracture; Post-traumatic superficial femoral AV fistula of same leg (ligated years previously) | Secondary | Left EIV | 8 × 5×6 cm3 | CT, MRI and fluoroscopic venogram and IVUS intra-operatively | Endovenous stent graft | Stent graft patent, no leak and no migration. Resolution of left leg swelling. Annual follow-up with Duplex. |
| Javaraj et al. [7] | 37F | Left gluteal pain | None | Primary | Left EIV | 3.6 cm | Duplex USS, CT and venography | Hybrid repair with open aneurysmectomy and primary closure over angioplasty balloon as a mandrel | Post-op venography showing no residual aneurysm. Well, at 4 months post-op. |
| Zou et al. [2] | 14F | Sudden-onset dyspnoea and syncope (PE) | None | Primary | Left EIV | Not stated | Duplex USS, CT | Mechanical fragmentation and low-molecular weight anticoagulant for PE. Surgery offered; family declined further treatment. | Asymptomatic at 16 months. |
Abbreviations: M = male; F = female; DVT = deep vein thrombosis; EIV = external iliac vein; CT = computed tomography; MRI = magnetic resonance imaging; post-op = post-operative; IIV = internal iliac vein; CIV = common iliac vein; IVC = inferior vena cava; USS = ultrasound scan; AV = aterio-venous; PE = pulmonary embolus; PSA = prostate specific antigen; IVUS = intravascular ultrasound.
The demographics, presentation, nature, location, size, imaging, management and outcome of iliac vein aneurysms reported in English since 2011 (PubMed search)
| Author . | Age and gender . | Symptoms . | Associated anomalies . | Primary or secondary? . | Location . | Size . | Imaging . | Management . | Outcome . |
|---|---|---|---|---|---|---|---|---|---|
| Fanshawe et al. 2017 (Current case) | 26M | Lower-urinary tract symptoms | DVT as a child | Secondary | Right EIV | 4 cm | CT, MRI and venography | Open aneurysmectomy with primary closure | Well, at 24 months post-op. CT confirming no residual aneurysm. Resolving lower urinary tract symptoms. |
| Audu et al. [1] | 63M | Left testicle and groin pain | Lower extremity varicose veins | Primary | Left IIV | 3.1 × 2.2 cm2 | MRI and venography | Endovenous embolisation | Symptom resolution at 1-month follow-up, with CT confirming aneurysmal occlusion. |
| Park et al. [4] | 63F | Acute severe abdominal pain | None | Primary | Right EIV | 4×5 cm2 | CT | Open aneurysmectomy with primary closure | Well, at months post-op, with Duplex USS every 6 months. |
| Shah et al. [8] | 22F | Incidental (found during work-up of bilateral acute limb ischaemia—treated with bilateral femoral embolectomies) | Patent foramen ovale; IVC obstruction; bilateral proximal common iliac stenoses | Primary | Right EIV | Not stated | CT | Open aneurysmorrhaphy with primary closure | Asymptomatic at 4-year follow-up, with surveillance Duplex USS demonstrating no recurrence. |
| Banzic et al. [9] | 24F | Non-healing skin ulceration below left knee | Misdiagnosis of Klippel–Trenaunay syndrome as a child; Right leg lengthening | Primary | Left CIV | 4 cm | CT, prior Duplex USS | Endovenous option presented; patient declined treatment. | Diagnosis of Parkes-Weber syndome (multiple AV fistulas throughout the left limb); Well at 2 years post diagnosis. |
| Escobar et al. [10] | 54F | Incidental (found during laparoscopic retroperitoneal dissection for endometrial adenocarcinoma) | None | Not stated | Right EIV | Not stated | Not performed | Not stated | Not stated. |
| Hosaka et al. [5] | 22F | Sudden-onset dyspnoea (PE) | None | Primary | Right EIV | 3.7 cm | CT | Open aneurysmectomy with great saphenous venous patch graft | Well, with patent EIV at 8-month follow-up. |
| Todorov et al. [6] | 62M | Incidental (elevated PSA) | Persistent left leg swelling following ankle fracture; Post-traumatic superficial femoral AV fistula of same leg (ligated years previously) | Secondary | Left EIV | 8 × 5×6 cm3 | CT, MRI and fluoroscopic venogram and IVUS intra-operatively | Endovenous stent graft | Stent graft patent, no leak and no migration. Resolution of left leg swelling. Annual follow-up with Duplex. |
| Javaraj et al. [7] | 37F | Left gluteal pain | None | Primary | Left EIV | 3.6 cm | Duplex USS, CT and venography | Hybrid repair with open aneurysmectomy and primary closure over angioplasty balloon as a mandrel | Post-op venography showing no residual aneurysm. Well, at 4 months post-op. |
| Zou et al. [2] | 14F | Sudden-onset dyspnoea and syncope (PE) | None | Primary | Left EIV | Not stated | Duplex USS, CT | Mechanical fragmentation and low-molecular weight anticoagulant for PE. Surgery offered; family declined further treatment. | Asymptomatic at 16 months. |
| Author . | Age and gender . | Symptoms . | Associated anomalies . | Primary or secondary? . | Location . | Size . | Imaging . | Management . | Outcome . |
|---|---|---|---|---|---|---|---|---|---|
| Fanshawe et al. 2017 (Current case) | 26M | Lower-urinary tract symptoms | DVT as a child | Secondary | Right EIV | 4 cm | CT, MRI and venography | Open aneurysmectomy with primary closure | Well, at 24 months post-op. CT confirming no residual aneurysm. Resolving lower urinary tract symptoms. |
| Audu et al. [1] | 63M | Left testicle and groin pain | Lower extremity varicose veins | Primary | Left IIV | 3.1 × 2.2 cm2 | MRI and venography | Endovenous embolisation | Symptom resolution at 1-month follow-up, with CT confirming aneurysmal occlusion. |
| Park et al. [4] | 63F | Acute severe abdominal pain | None | Primary | Right EIV | 4×5 cm2 | CT | Open aneurysmectomy with primary closure | Well, at months post-op, with Duplex USS every 6 months. |
| Shah et al. [8] | 22F | Incidental (found during work-up of bilateral acute limb ischaemia—treated with bilateral femoral embolectomies) | Patent foramen ovale; IVC obstruction; bilateral proximal common iliac stenoses | Primary | Right EIV | Not stated | CT | Open aneurysmorrhaphy with primary closure | Asymptomatic at 4-year follow-up, with surveillance Duplex USS demonstrating no recurrence. |
| Banzic et al. [9] | 24F | Non-healing skin ulceration below left knee | Misdiagnosis of Klippel–Trenaunay syndrome as a child; Right leg lengthening | Primary | Left CIV | 4 cm | CT, prior Duplex USS | Endovenous option presented; patient declined treatment. | Diagnosis of Parkes-Weber syndome (multiple AV fistulas throughout the left limb); Well at 2 years post diagnosis. |
| Escobar et al. [10] | 54F | Incidental (found during laparoscopic retroperitoneal dissection for endometrial adenocarcinoma) | None | Not stated | Right EIV | Not stated | Not performed | Not stated | Not stated. |
| Hosaka et al. [5] | 22F | Sudden-onset dyspnoea (PE) | None | Primary | Right EIV | 3.7 cm | CT | Open aneurysmectomy with great saphenous venous patch graft | Well, with patent EIV at 8-month follow-up. |
| Todorov et al. [6] | 62M | Incidental (elevated PSA) | Persistent left leg swelling following ankle fracture; Post-traumatic superficial femoral AV fistula of same leg (ligated years previously) | Secondary | Left EIV | 8 × 5×6 cm3 | CT, MRI and fluoroscopic venogram and IVUS intra-operatively | Endovenous stent graft | Stent graft patent, no leak and no migration. Resolution of left leg swelling. Annual follow-up with Duplex. |
| Javaraj et al. [7] | 37F | Left gluteal pain | None | Primary | Left EIV | 3.6 cm | Duplex USS, CT and venography | Hybrid repair with open aneurysmectomy and primary closure over angioplasty balloon as a mandrel | Post-op venography showing no residual aneurysm. Well, at 4 months post-op. |
| Zou et al. [2] | 14F | Sudden-onset dyspnoea and syncope (PE) | None | Primary | Left EIV | Not stated | Duplex USS, CT | Mechanical fragmentation and low-molecular weight anticoagulant for PE. Surgery offered; family declined further treatment. | Asymptomatic at 16 months. |
Abbreviations: M = male; F = female; DVT = deep vein thrombosis; EIV = external iliac vein; CT = computed tomography; MRI = magnetic resonance imaging; post-op = post-operative; IIV = internal iliac vein; CIV = common iliac vein; IVC = inferior vena cava; USS = ultrasound scan; AV = aterio-venous; PE = pulmonary embolus; PSA = prostate specific antigen; IVUS = intravascular ultrasound.
Iliac vein aneurysms may be primary or secondary, in association with previous trauma or vascular malformation syndromes, e.g. Parkes-Weber [3]. In this case, the iliac vein aneurysm was secondary and most likely developed as a result of iatrogenic vascular trauma (multiple femoral central venous catheters) in the neonatal period. Iliac vein aneurysms can be difficult to diagnose and the differential may include groin hernias or lymphadenopathy. They are often asymptomatic, but may present with thomboembolism or, rarely, abdominal pain. This is the first reported case of an iliac vein aneurysm presenting with lower urinary tract symptoms. Investigations of choice include CT (venous phase), real-time venography and MRI. All three were used in the case presented.
Complications associated with iliac vein aneurysms include rupture [4] and thromboembolism. Primarily to prevent thromboembolism, operative management has been hitherto recommended. Operative strategies include excision, with or without interposition grafting, or tangential excision—as in the case we present here—with or without patch repair, if residual vessel calibre or wall fragility is a concern. Hosaka et al. [5] used a dual saphenous vein patch in their operative technique. Endovenous strategies of both stent grafting and embolisation have also been employed with success [1, 6]. Javaraj et al. [7] also performed a successful hybrid procedure in 2012.
The rarity of vein aneurysms, together with the heterogeneity of presentation, investigation and management make it difficult to draw meaningful conclusions regarding their optimal treatment. This case is the first reported of an EIV aneurysm presenting with lower urinary tract symptoms, due to a compressive effect on the bladder.
ACKNOWLEDGEMENTS
None declared.
CONFLICT OF INTEREST STATEMENT
None declared.



