-
PDF
- Split View
-
Views
-
Cite
Cite
Adam Loutfy, Sugam Vasani, Locally advanced colon cancer resulting in en bloc right hemicolectomy and pancreaticoduodenectomy: case report and review of literature, Journal of Surgical Case Reports, Volume 2018, Issue 5, May 2018, rjy100, https://doi.org/10.1093/jscr/rjy100
Close - Share Icon Share
Abstract
Locally advancement of right colon cancer to the surrounding organs requiring surgical intervention is an extensive procedure associated with numerous risks. There are not many cases of which this phenomenon may occur. En bloc pancreaticoduodenectomy and resection of involved viscera should be considered for patients who can appropriately undergo this exhaustive surgery. Our objective is to report the experience we had with this patient who underwent an en bloc pancreaticoduodenectomy and right hemicolectomy and review literature. Our method was a retrospective review of a patient with colon cancer
INTRODUCTION
Locally advanced colorectal cancer has beneficial treatment via en bloc pancreaticoduodenectomy and right hemicolectomy. The morbidity and mortality rates are acceptable with an experienced team. More often than not, excluding patients who are not surgical candidates due to various comorbidities, en bloc pancreaticoduodenectomy and right hemicolectomy should be performed for locally advanced colorectal cancers. Bias does exist for numerous reasons but the most important being a lack of enrollment of patients.
CASE REPORT
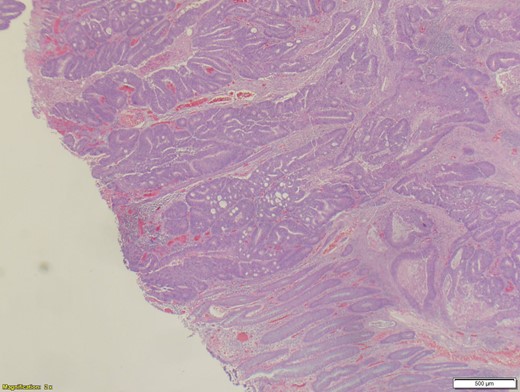
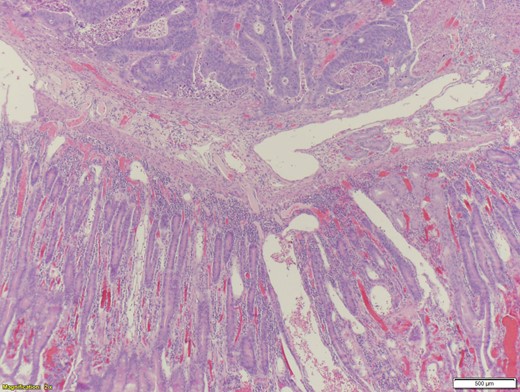
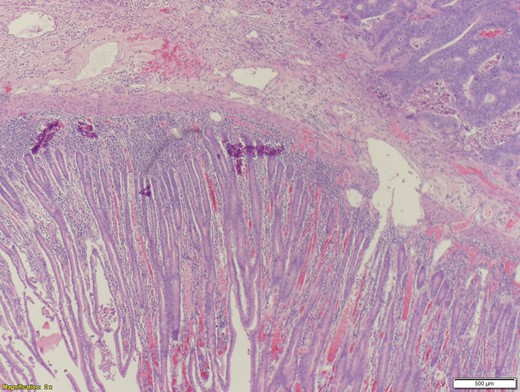
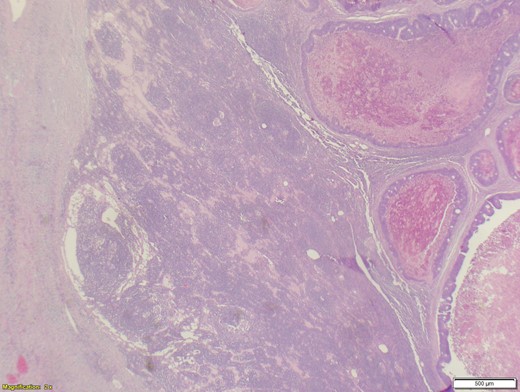
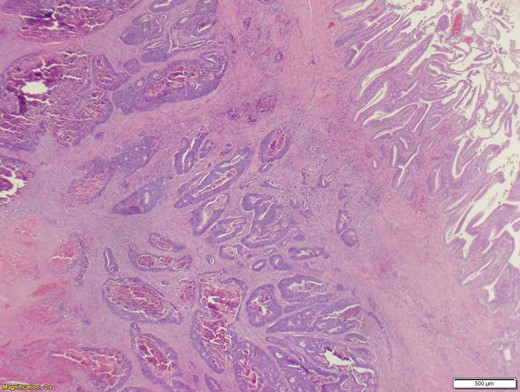
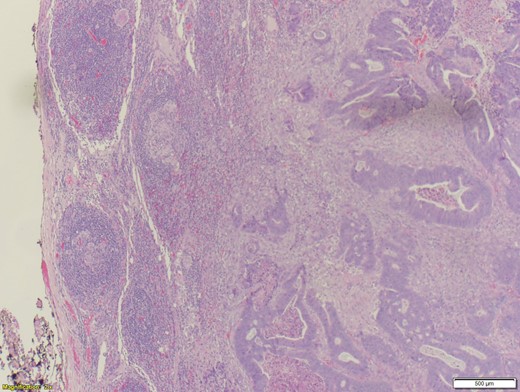
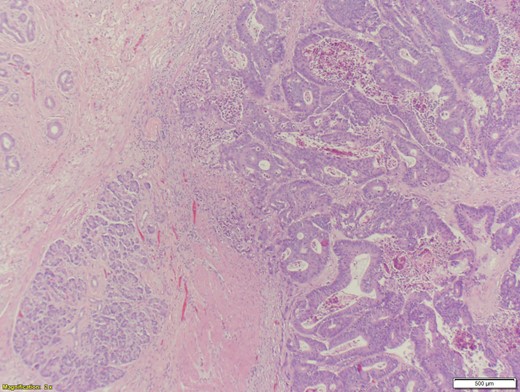
A 70-year-old female presented to the emergency department with complaints of diarrhea, vague, dull abdominal pain, unintentional weight loss and poor appetite. No hematochezia or melaena stated. Fecal occult is strongly positive in the ED. No endoscopies were found in her records. PMHx included COPD, osteoarthritis and DVT. Significant physical exam findings included mild, diffuse abdominal tenderness and RUQ palpable mass, and normal bowel sounds. Labs were significant for a hemoglobin of 5.7, hematocrit of 18.6% and CEA of 29.6. An abdominal/pelvis CT exhibited a 6 cm circumferential mass of the hepatic flexure (Figs 1–3). Two days later, a right hemicolectomy with en bloc pancreaticoduodenectomy was performed. Pathology showed adenocarcinoma stage IIIc (Figs 4–10). Post-operatively, an abdominal/pelvis CT showed bilateral pulmonary emboli and a 14 cm pelvic abscess. Bilateral lower extremity ultrasound showed low probability for DVT. Exploratory laparotomy was performed where the pelvic abscess was seen and extensive lysis of adhesions, resection of ileocolonic anastomosis for contained leak and ileostomy performed. Approximately 4 months after discharge, the patient passed away while in a long-term care facility.



DISCUSSION
Locally advanced colon cancers to adjacent organs have been a rare phenomenon. However, recently, ~5.2–23.6% of all colorectal cancers, at the time of presentation, penetrate or adhere to adjacent organs [1]. Even less have been discovered to invade the duodenum and/or pancreas [2]. In previous years, invasion of colorectal cancers were considered unresectable [2]. As research progresses, it has been proven that there has been a decrease in mortality rates with resection of the tumor and involved adjacent organs [3]. Due to a lack of visualization, local metastatic colorectal cancers are often identified at the time of surgical exploration, in which the surgeon may not be completely prepared to resect such a complex spread of cancer. However, we believe that with an experienced team, post-operative mortality and morbidity rates of right hemicolectomy with en bloc pancreaticoduodenectomy are considerably lower than other methods of treatment.
When it comes to surgical intervention, there are three main methods of management of locally invasive colorectal cancers. These include hemicolectomy along with either en bloc pancreaticoduodenectomy, partial duodenectomy with either a pedicled ileal flap repair or direct suture. A 1947 study presented by Calmenson e Black, included a series of eight patients whom had locally advanced colon cancer with duodenal invasion. These patients agreed to a duodenal resection that resulted in a 0% survival rate after a year (three dying immediately in the post-operative period) [4]. The first case of right hemicolectomy with en bloc pancreaticoduodenectomy was described by Van Prohaska in 1953 [5]. Evidence shows that aggressive resection of adjacent organs along with a hemicolectomy has acceptable morbidity and mortality rates [6]. In comparison, a partial duodenal wall resection was associated with a poor outcome [7]. Even though complete resection remains controversial, microscopic examination of locally advanced colorectal cancers have shown to have a direct extension through the serosa of adjacent organs in 53.4%, whereas the remaining 46.6% showed a simple inflammatory adherence [8]. Since over 50% of locally advanced colorectal cancers resulted in a microscopic infiltration, a right hemicolectomy plus pancreaticoduodenectomy is strongly recommend for tumors that invade or are suspected to invade the duodenum and/or the pancreas [3]. However, when limited to the duodenum, a local duodenal resection is sufficient [9]. When an R0 resection was possible (achievable in 93% of all colorectal cancers), a poor outcome was avoided. However, patients with R1 or R2 resection have a 0% 5-year survival rate, compared to the 80.7% in R0 resection patients [8]. The greatest factor in the survivability of locally advanced colorectal cancer patients is when R0 resection is possible, as confirmed by Lehnert et al. [6]. Advanced age alone, apart from usually associated comorbidities, is not considered an absolute contraindication to multivisceral resection, considering the better overall results as opposed to more conservative approaches [1].
A 2013 study showed that patients who are appropriate for right hemicolectomy with en bloc pancreaticoduodenectomy have the following characteristics: ‘(i) no distant metastasis, (ii) R0 resection being possible on the basis of the preoperative examination, (iii) the patient’s condition being good enough to accept radical multivisceral resection and (iv) the surgical team being experienced enough to perform the procedure’ [10]. Preoperative evaluations are strongly recommended to ensure that patients qualify. Preoperative staging is also a key factor; this is done through abdominal CT scans. CT scans have a significant (99%) ability to detect liver metastases, moderate ability to reveal cT4 stage (86%) cancers but are poor at detecting peritoneal carcinomatosis [10]. CTs are able to distinguish colonic tumor stages pre-operatively and can show invasion through the muscularis propria, indicating stage T3/T4 [10].
Potential complications can occur post-operatively. A 2014 study showed, within a 30-day post-operative period, morbidity rates were 12.8% (5 out of 39 patients) with en bloc pancreaticoduodenectomy and hemicolectomy, 12.5% (one out of eight patients) with pedicled ileal flap repair, and 0% with duodenal resection with direct suture. Pancreatico-jejunal anastomotic leak was frequently seen as a major complication after a pancreaticoduodenectomy with en bloc right hemicolectomy (3 out of 39 patients) [2]. A 1944 study by Linton described two cases with duodeno-colic fistula complications post-operatively [7]. None of the series in the former 2014 study reported a 30-day post-operative mortality rate.
A study suggested that only successful cases were presented as well as rejection of patients from outpatient clinics. Secondly, few studies provided sufficient analysis of patients who purely underwent en bloc pancreaticoduodenectomy and right hemicolectomy. Finally, each study had their own indications for en bloc multivisceral surgery that differ from the next. This is a possible explanation as to why reported percentages of carcinomatous adhesions ranged from 47.2 to 100% [3].
CONFLICT OF INTEREST STATEMENT
None declared.



