-
PDF
- Split View
-
Views
-
Cite
Cite
José Raúl Guerra-Mora, Ulises Bravo-Ángel, Rodrigo Efraín Hernández-Reséndiz, Rosa María Vicuña-González, Jessica Frías-Guillén, Irina Jeanette Bercholc-Urinowsky, Carlos Cesar Bravo-Reyna, Ulises García-González, Anaplasic astrocytoma with exophytic growth in Sylvian fissure in a pediatric patient: a case report, Journal of Surgical Case Reports, Volume 2018, Issue 4, April 2018, rjy079, https://doi.org/10.1093/jscr/rjy079
Close - Share Icon Share
Abstract
Gliomas are the most frequent supratentorial intracranial tumors in the pediatric population. Usually, they are intra-axial lesions with a characteristic image pattern, however, there are few reported cases of gliomas with exophytic growth. There are no previous reports in the literature of gliomas with exophytic growth in the Sylvian fissure. Fourteen year-old female patient who started with seizures. In imaging studies, a neoplasic mass with an exophytic portion in the left Sylvian fissure was found. Macroscopically, total resection was performed, definitive diagnosis was anaplastic astrocytoma. She presented recurrence and is currently receiving adjuvant treatment. Supratentorial gliomas with exophytic growth are extremely rare. We report the first case in the pediatric population, and we consider it is important to know its imaging and macroscopic characteristics for its initial management and to take it into account as a differential diagnosis of exophytic lesions.
INTRODUCTION
Intracranial tumors have an annual incidence of 3/100 000 cases in the pediatric population, this makes it one of the most frequent causes of death in this age group [1]. Astrocytomas are the most common intracranial tumors in the pediatric population, accounting for up to one-third of supratentorial neoplasms. The most common imaging features include the following characteristics: heterogeneous mass, cystic with solid portions, heterogeneous contrast enhancement [1]. The vast majority of astrocytomas are intra-axial, however, they may have exophytic growth which can resemble other intracranial neoplasms in the image. The exophytic growth of gliomas is well known in the brainstem, however, there are few reports of cases from other locations, such as cerebellopontine angle [2], cerebellum [3] and brainstem [4]. To our knowledge, there is no previous report of any case of anaplastic astrocytoma with exophytic growth at the Sylvian fissure level in the pediatric population. The knowledge of this type of presentation is important to be taken into account as a differential diagnosis of masses with exophytic growth, besides its behavior and prognosis regarding purely intra-axial gliomas remains unknown.
CASE REPORT
A 14-year-old female with no relevant medical history was referred to the emergency department for the presence of one episode of generalized tonic–clonic seizure lasting ~2 min, with 30 min of postictal state. At the time of the evaluation, she was asymptomatic. The physical examination showed a Glasgow coma scale of 15 points, pupils 3 mm diameter, facial symmetry, muscular strength 5/5 in the four limbs, the rest was normal. A simple computerized tomography and magnetic resonance imaging of the brain were requested, which showed a neoplastic lesion with an exophytic component at the level of the Sylvian fissure (Fig. 1).
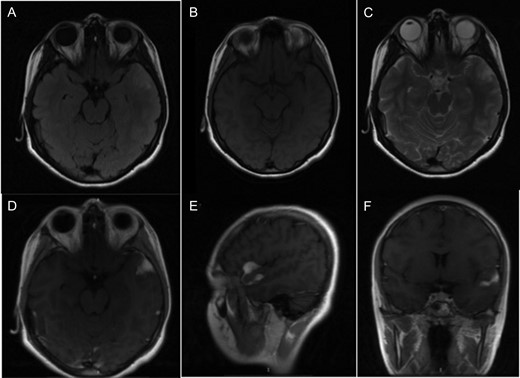
(A) T2 flair sequence showing a slightly hyperintense lesion. (B) Lesion behaves isointense to brain parenchyma in T1 sequence. (C) Hyperintense in T2 sequence. (D–F) Axial, sagittal and coronal images, respectively, with contrast enhancement of the tumor.
A classic pterional approach was performed, we found a multilobulated and vascularized mass with exophytic component at the level of the left Sylvian fissure (Fig. 2). A macroscopic total resection was performed, with abundant hemorrhage (900 mL). At the follow up the next month, she got 90 points in the Karnofsky scale.

Macroscopic image of the tumor. Exophytic growth can be seen with the involvement of the arachnoid plane at the level of the Sylvian fissure.
The histopathological study showed anaplastic astrocytoma. In the immunohistochemistry reactions, there was intense positivity for the glycoprotein acid protein, negativity for the epithelial membrane antigen, a Ki67 with a proliferation index of 5% and a p53 positive in 30% of the neoplastic cells (Fig. 3).
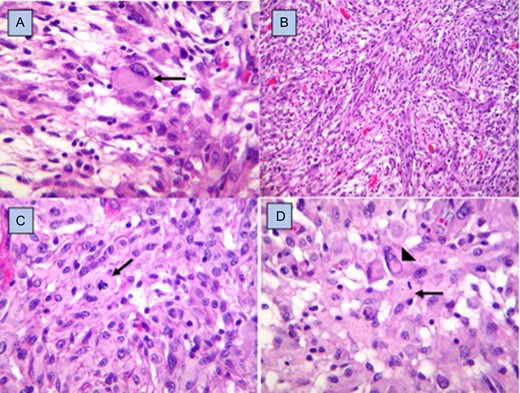
Histopathology. Fibrillar matrix with pleomorphic cells, some with gemistocytic appearance (arrow) (A), alternating with areas of spindle cells arranged in interlaced fascicles (B), and round cells with epithelioid appearance (C), with mitosis figures (arrows), as well as others with nuclear atypia and pseudointranuclear inclusions (arrowhead) (D). Hematoxylin and eosin staining, ×40.
Treatment consisted in radiotherapy and chemotherapy. The 33 sessions of radiotherapy with 59.4 Gy, and chemotherapy with carboplatin, vincristine and temozolomide. After 8 months of treatment, the tumor recurred; for that reason, nimotuzumab was added to treatment (Fig. 4).
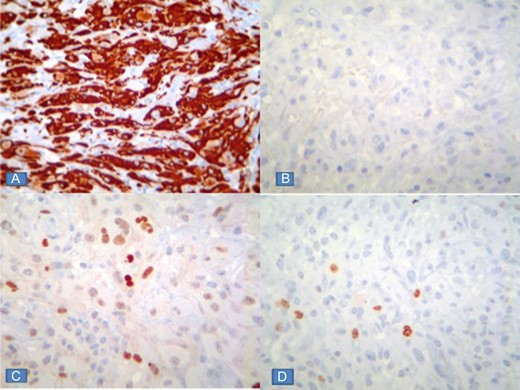
Immunohistochemical reactions showing intense positivity for gliofibrillary acid (A) protein, negativity for epithelial membrane antigen (B), p53 positivity in 30% of neoplastic cells (C), and Ki67 proliferation index of 5% (D).
DISCUSSION
Neuroimaging studies are an indispensable tool in the diagnosis of intracranial lesions, suspicion of the type of tumor is based on the epidemiological characteristics, lesion location and contrast enhancement patterns, but when there is an unusual lesion, the diagnosis becomes a challenge.
The term exophytic refers to lesions that meet the following two criteria: (i) Observation in preoperative magnetic resonance imaging studies outside the anatomic limits of the brain surface and (ii) trans-surgical identification of pial and arachnoid invasion, with tumor growth through cisterns [5]. There are sporadic reports in adults about astrocytic lesions of a high degree of exophytic behavior [6, 7], and few series of isolated cases in the pediatric population, in which their location has been infratentorial.
The present work corresponds to the first report of anaplastic astrocytoma with exophytic behavior with supratentorial localization. Its behavior has been of rapid progression despite achieving macroscopically complete resection and adjuvant therapy with chemotherapy and radiotherapy, which is one of the hallmarks of high-grade tumors in the pediatric patient [8].
According to the tumor growth and dissemination patterns described by Yasargil and other authors [7, 9, 10], the growth of this tumor does not follow a pattern previously described in limbic or paralimbic gliomas, which in addition to the aforementioned highlights the importance to be reported.
CONCLUSION
The presence of supratentorial gliomas with exophytic growth is extremely rare and even more so in the Sylvian fissure. We report the first case of an anaplastic astrocytoma with exophytic growth at the Sylvian fissure in pediatric population, so we could consider it as a differential diagnosis of extra-axial lesions at Sylvian fissure.
Conflict of Interest statement
None declared.



