-
PDF
- Split View
-
Views
-
Cite
Cite
A Gardner, J Sahota, H Dong, V Saraff, W Högler, N J Shaw, The use of magnetically controlled growing rods in paediatric Osteogenesis Imperfecta with early onset, progressive scoliosis, Journal of Surgical Case Reports, Volume 2018, Issue 3, March 2018, rjy043, https://doi.org/10.1093/jscr/rjy043
Close - Share Icon Share
Abstract
Osteogenesis Imperfecta (OI) is a condition of bone fragility and can present with early onset scoliosis that can cause respiratory complications in later life. The fear of instrumenting the spine in OI is the possibility of fracture either on primary insertion or subsequent lengthening. Magnetically controlled growing rods were inserted to control a scoliosis in a 6-year old with OI type IV. Fixation was obtained using pedicle screws proximally and distally with sublaminar bands around the ribs proximally. These rods have been remotely lengthened on multiple occasions over a 2-year period. This has controlled the scoliosis whilst also allowing the spine to grow. There are no complications to report. This case reports the use of magnetically controlled growth rods used to manage early onset scoliosis in OI. Frequent lengthening, achieving small increases in length on every occasion protects against the risk of fracture during the lengthening procedure.
INTRODUCTION
Osteogenesis Imperfecta (OI) is a condition of reduced bone quality presenting with many features including bone fragility, deformity and scoliosis. Classically, severe and progressive scoliosis in OI is managed conservatively until definitive fusion can be performed [1, 2] allowing maximum correction of the deformity with further prevention of progression.
Scoliosis of any aetiology, 10 years or under is classified as early onset scoliosis [3]. Management is non-operative through observation and bracing, or operative with technologies allowing spinal growth with deformity correction. Originally, this was done using traditional growing rods (TGR) although recently other technologies have become available [4].
Growing rods have now been developed which can be lengthened remotely. In the UK, the National Institute for Health and Care Excellence [5] has mandated that the Magnetically Controlled Growth Rod (MCGR, Nuvasive, San Diego, CA, USA) is used where clinically appropriate. To date, the usefulness of this technology in an OI patient has not been demonstrated. We report a prepubertal girl with OI type IV treated with an MCGR system for early onset scoliosis.
CASE REPORT
The girl was diagnosed with OI when she presented with bilateral femur fractures at the age of 9 months. Phenotypically she had OI Type IV. Genetic testing identified a mutation in Exon 8 of COL1A1 (c.608G > T;p.Gly203Val).
She had been on bisphosphonate therapy from the age of 1 year, initially with intravenous Pamidronate every 3 months, followed from the age of 3.5 years by intravenous Zoledronate every 4 and later every 6 months [6]. Her major clinical problem over that time was constipation requiring a regular osmotic laxative.
She had gross motor delay and did not walk until the age of 3.5 years. She was noted to have scoliosis from the age of 20 months, which was managed conservatively until noted to be worsening aged 4 years. The scoliosis was a double major pattern (Cobb angle of 32° in the thoracic spine and 35° in the thoracolumbar spine). A whole spine MRI and CT revealed a normal neural axis with no evidence of abnormal bone architecture, basilar invagination or spondylolisthesis.
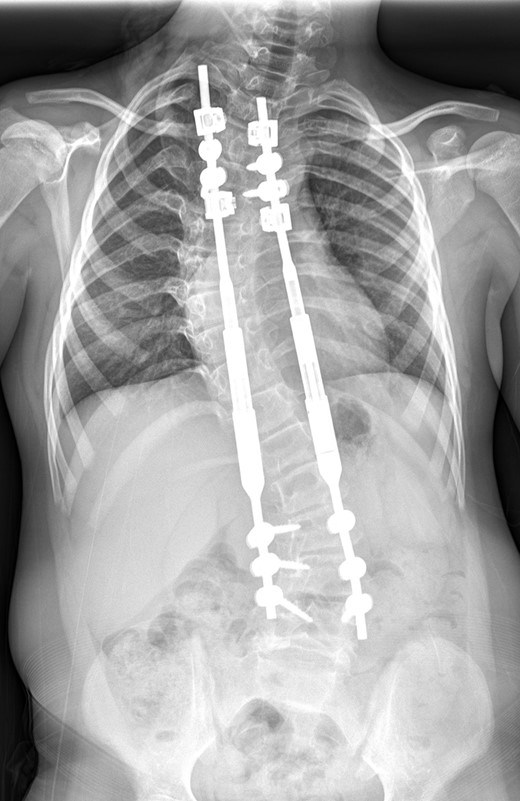
Between the ages of 4 and 6 years, the curve increased rapidly leading to a significant curve measuring 80° in the thoracic spine and 65° in the thoracolumbar spine with a T1–S1 height of 232 mm and T1–T12 height of 150 mm (Fig. 1). A decision was made to intervene operatively and posterior instrumentation with MCGR was performed. Special consideration was given to her bone fragility. Following 4.5 years of bisphosphonate therapy, her last bone mineral density (BMD) assessment by dual energy X-ray absorptiometry before surgery was normal. Her lumbar spine BMD Z-score was +1.5 and the total body less head BMD Z-score was also +1.5. Thus, at age 6 years, a construct of three paired sets of pedicle screws were placed at L2–L4 distally and a combination of pedicle screws at two levels (T4 and T5), with an outer square of sublaminar bands passed under the third and sixth ribs, was placed proximally. The instrumentation used was a 4.5 Expedium System (DePuy Synthes, Raynham, MA, USA) and the Silc Sublaminar Banding System (Globus Medical, Audubon, PA, USA). Post-operative radiographs (Fig. 2) showed good spinal balance and correction of deformity, but fractures of the right 5th and 10th ribs were seen posteriorly at the junction of the rib and transverse process. Following 8 weeks of spinal cast jacket protection, a CT scan showed the rib fractures to have healed. After instrumentation the thoracic curve angle measured 38° and the thoracolumbar curve measured 30°, with a T1–S1 height of 247 mm and a T1–T12 height of 160 mm.
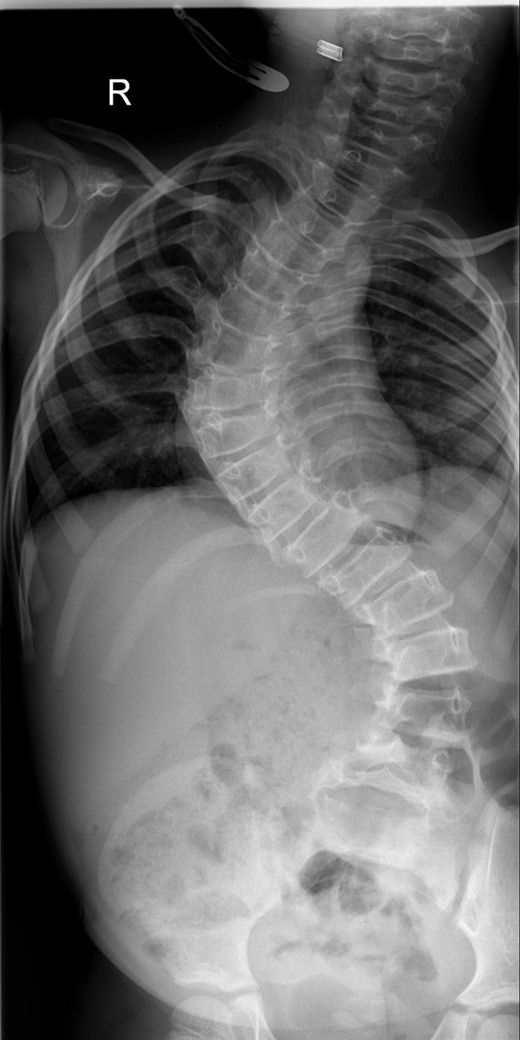
A whole spine radiograph at age 6 demonstrating the double major scoliosis (measuring 80° in the thoracic curve and 65° in the thoracolumbar curve with a T1–S1 height of 232 mm and T1–T12 height of 150 mm).

An immediate post-operative whole spine radiograph demonstrating the spinal construct with the MCGR rods (measuring 38° in the thoracic curve and 30° the thoracolumbar curve with a T1–S1 height of 247 mm and a T1–T12 height of 160 mm).
Subsequent transcutaneous, magnetic spinal lengthening has been performed on six occasions in the outpatient setting over the last 2 years. This has been uncomplicated and has not been associated with significant pain or fracture. She takes paracetamol after each magnetic lengthening procedure, easing mild muscular discomfort. The control of the scoliosis has been maintained, and at 2 years post-insertion of MCGR the spinal curves now measure 40° for the thoracic curve and 37° for the thoracolumbar curve with a T1–S1 height of 288 mm and T1–T12 height of 195 mm (Fig. 3). The MCGR have been lengthened by 16 mm on either side.
A whole spine radiograph at age 8 following multiple lengthening procedures showing elongation of the MCGR rods (measuring 40° for the thoracic curve and 37° for the thoracolumbar curve with a T1–S1 height of 288 mm and T1–T12 height of 195 mm).
Since the spinal surgery, there have been no spine-related problems and no issues with constipation. The girl has sustained femoral shaft fractures secondary to minimal trauma that led to bilateral femoral nailing using Fassier Duval telescopic, intramedullary nails (Pega Medical, Laval, Quebec, Canada).
DISCUSSION
OI is known to be associated with scoliosis [7]. In some cases, scoliosis develops at an early age and is labelled ‘early onset scoliosis’ [3]. For such cases, instrumentation that allows both control of the curve and spinal growth is required. Whilst TGRs have been used for patients with early onset scoliosis, fear of fracture at the foundations of the construct during lengthening means that this has not been used in the OI group.
In contrast to TGR, the MCGR allows frequent lengthening procedures of a small amount. Frequent lengthening means less force is required to achieve an increase in the length of the construct at each procedure making MCGR a more attractive option over TGR in the OI child. This case report demonstrates the success of MCGR for controlling the scoliosis with continued growth of the spine following transcutaneous magnetic rod lengthening over 2 years post-insertion. Extra care was taken when placing the bony anchors for this construct given the risk of fracture. It was felt that sublaminar bands around the ribs at the proximal end of the construct would aid in preventing proximal junctional failure or screw pull out.
This case illustrates the successful use of the MCGR for early onset scoliosis in OI, with good outcome at two years.
Written informed consent was obtained from the patient’s legal guardian(s) for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
ACKNOWLEDGEMENTS
Not applicable.
CONFLICT OF INTEREST STATEMENT
None of the authors have any competing interests to declare.
FUNDING
There are no funding sources to acknowledge.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This case report is of standard care and thus there is no requirement for ethical approval. Consent for the procedure was taken following the policies and procedures of the host institution.
CONSENT FOR PUBLICATION
Written permission for publication was given.
AVAILABILITY OF DATA AND MATERIAL
All data generated or analysed during this study are included in this published article [and its supplementary information files].
AUTHORS CONTRIBUTIONS
A.G. performed the case and all of the lengthening procedures. J.S., V.S., W.H. and N.S. provided guidance on the condition and contributed to the article. H.D. contributed to the literature review. All authors have read and approved the final article.



