-
PDF
- Split View
-
Views
-
Cite
Cite
Heena S Chotai, Guy Finch, Davis Thomas, Gabor Libertiny, Successful management of an aorto-gastric fistula occurring 15 years after oesophagectomy with covered aortic stent graft placement followed by open surgery, Journal of Surgical Case Reports, Volume 2018, Issue 2, February 2018, rjy019, https://doi.org/10.1093/jscr/rjy019
Close - Share Icon Share
Abstract
Aorto-gastric fistula (AGF) is an uncommon and life threatening complication of oesophagectomy. Usually occurring in the immediate weeks following the procedure at anastomosis lines, this case describes a rare development of an AGF 15 years after an oesophagectomy due to the presence of a benign ulcer. Initially successful endovascular stenting of the thoracic aorta was followed by re-bleed, further stenting but eventually open surgery was required.
INTRODUCTION
A fistula between the thoracic aorta and a pulled-up stomach (neo-oesophagus) after oesophagectomy is an uncommon and often fatal complication causing massive haemorrhage.
Most previous cases documented the development of fistulae at suture or anastomosis lines penetrating or perforating into the aorta [1–3]. This is usually seen within weeks of the procedure and likely as a complication of acute infection or leak [1, 3, 4].
We describe the management of a patient with AGF that developed due to benign ulceration 10 years after oesophagectomy for cancer. Initially we carried out thoracic aortic endovascular stenting, then due to a re-bleed repeated stenting was followed by open surgery.
(The case and images have been consented for use in publication by the patient.)
CASE REPORT
A 57-year-old male presented haemodynamically unstable with a blood pressure of 85/50 mmHg and a heart rate of 136 bpm with haematemesis, melaena and 4-day history of back pain. Fifteen years previously he was treated for a poorly differentiated adenocarcinoma (pT3 pN1 MX) close to the gastro-oesophageal junction with chemotherapy and trans-hiatal oesophagectomy. He received no radiotherapy. Apart from being a life-long smoker he had no other positive social risk factors or medical history. He underwent immediate oesophago-gastro-duodenoscopy (OGD). This showed fresh and clotted blood in the gastric remnant but no bleeding source was identified. He had a pulseless arrest during the OGD but underwent successful cardiopulmonary resuscitation. Following this a CT angiogram was performed. This demonstrated a fistula between the neo-oesphagus and the thoracic aorta (Fig. 1). Following discussion between an upper gastro-intestinal surgeon, a vascular surgeon and an interventional radiologist the patient was taken to the operating theatre. Under general anaesthesia an initial thoracic aortogram was performed from the right groin to confirm the presence and location of the AGF (Fig. 2). Following this, a covered thoracic stent graft (Cook Medical ZTA-24-105/diameter of 24 mm and length of 105 mm), was inserted via the femoral artery under image guidance. The stent graft, usually used in aneurysmal repair, was placed in the thoracic aorta across the fistula and occluded it. Subsequent angiogram showed no leak (Fig. 3). The patient became haemodynamically stable and had an uneventful recovery.
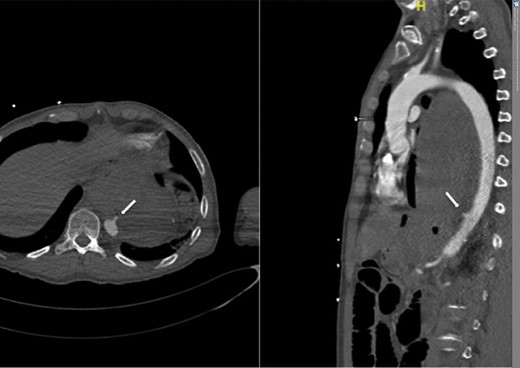
CT angiogram showing aorta-enteric fistula demonstrated by arrow (axial and sagittal view, respectively).
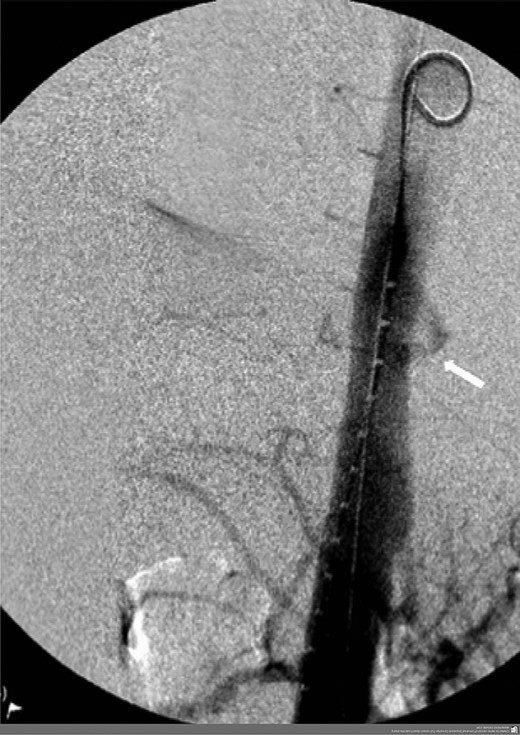
Angiogram prior to primary aortic stenting; leak via fistula demonstrated by arrow.

A week later, he underwent a further OGD. This showed a benign ulcer (Fig. 4), which was later confirmed histologically. Helicobacter pyloriwas negative. He was discharged home 8 days post stent insertion with a further 2-week course of co-amoxiclav (Amoxicillin/clavulanic acid) and 1 week of fluconazole, as recommended by a consultant microbiologist, and life-long omeprazole. He remained well for the next months.
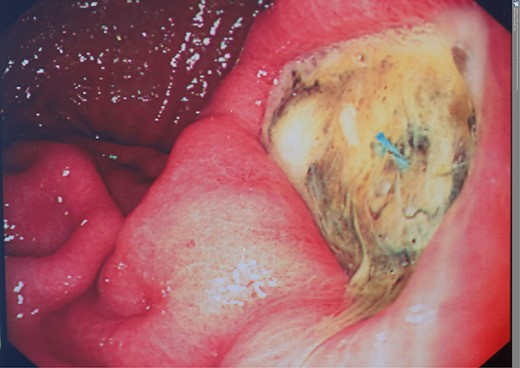
However, 4 and a half months later he again became haemodynamically unstable with a further episode of haematemesis. A further CT angiogram showed contrast entering the neo-oesophagus from the thoracic aorta (Fig. 5). The patient was again taken to the emergency theatre and the previous stent was relined with further stents extending both proximally and distally beyond the previous stent, with care taken not to occlude the celiac trunk and arteries below this (Cook Medical ZTA-26-105 and Cook Medical ZTA-28-109). Again, the patient had a quick recovery. However, repeat endoscopy showed that the aortic stent was visible through a defect in the wall of the neo-oesophagus (Fig. 6).
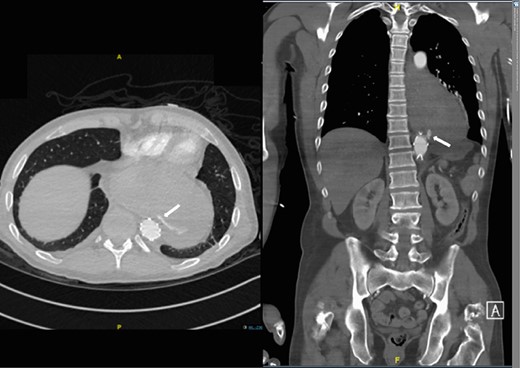
Second admission: CT angiogram showing aorta-enteric fistula demonstrated by arrow (axial and sagittal view, respectively).
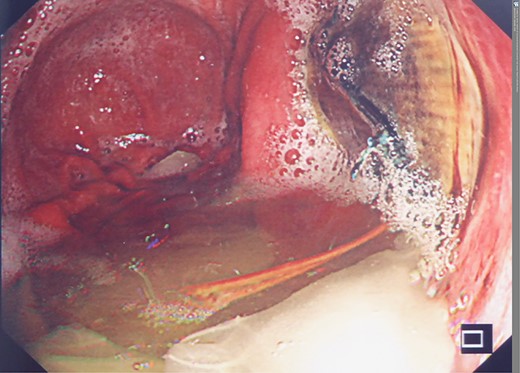
Second admission: OGD post second stent insertion demonstrating visibility of aortic stent via defect in wall of neo-oesphagus.
At this point the patient was referred to the Liverpool Thoracic Aneurysm Service where he underwent a left thoracotomy. The thoracic aorta was clamped proximal and distal to the aortic stents and a left heart bypass was established for distal perfusion. The aorta was opened, the stents excised and replaced with a 22 mm Dacron tube graft. After mobilizing the neo-oesophagus from the aorta, the edges of the defect, which appeared clean and healthy, was repaired directly. A week later contrast swallow showed satisfactory repair of the neo-oesophagus with no anastomotic leak.
The removed aortic stents grew candida albicans sensitive to Fluconazole. The patient continues on antibiotics, including antifungals. He remains well and is due to undergo treatment for his extensively carious teeth.
DISCUSSION
AGF is an uncommon and often lethal complication of previous oesophagectomy. It may present within weeks after surgery [5] due to anastomotic problems or later, due to recurrent malignancy [5]. Our patient had no sign of malignancy for over a decade. Radiotherapy, though not a factor in this case, can also contribute to the breakdown of soft tissue planes in the irradiated field [5].
In the absence of other predisposing factors and in the presence of a previous truncal vagotomy that was part of the original oesophagectomy, smoking may have contributed to the development of a benign ulcer in the pulled-up gastric remnant, adhering to and then eroding into the aorta.
The treatment for AGF is difficult. Conservative treatment commonly fails with inevitable death [5]. In some patients, with recurrent malignancy, palliation may have a role. Formal open repair through thoracotomy has been considered definitive treatment but carries a high risk of mortality even in specialized institutions in the acutely unwell patient.
Our patient was treated initially by endovascular means using a covered thoracic aortic stent graft, normally used in aneurysmal repair. Infection and/or mechanical pressure from this resulted in the failure of this treatment and open repair became necessary. However, the initial stenting meant that this major operation could be carried out in a stable patient who was systemically well. This is likely to have contributed to a satisfactory outcome. Ongoing concern remains regarding recurrent graft infection. Life-long surveillance, prolonged antibiotic treatment and abolishing likely septic sources are necessary to reduce this risk.
Our experience points towards the temporizing role of aortic stent-grafts in patients with AVG but, due to the lack of trials, treatment for these difficult patients has to be tailored individually.
CONFLICT OF INTEREST STATEMENT
None declared.



