-
PDF
- Split View
-
Views
-
Cite
Cite
David N Holmes, Lara Armstrong, James Bennett, H Neil Simms, Neurosurgical management of multiple intracranial Nocardia and Enterococcus abscesses in an immunocompetent patient, Journal of Surgical Case Reports, Volume 2018, Issue 2, February 2018, rjy015, https://doi.org/10.1093/jscr/rjy015
Close - Share Icon Share
Abstract
Nocardia farcinica and Enterococcus faecium are both rare causes of cerebral abscess. The former is associated with high morbidity and mortality. We describe a neurosurgical approach to the management of multiple intracranial abscesses of dual microbial pathology in an immunocompetent patient to achieve a good outcome.
INTRODUCTION
Nocardia species account for ~2% of all cerebral abscesses [1]. This most often presents following opportunistic infection of an immunosuppressed patient. Cerebral abscess formation in the immunocompetent patient is therefore less well-described. Cerebral abscesses of an Enterococcus aetiology are similarly rare and predisposing factors are often found. The largest case series numbers 12 patients with only 10 cases identified in the preceding literature [2]. The rarity of these cases and lack of prospective, randomized data means the optimum therapeutic strategy is often unclear. This case report presents the clinical course and management of a patient with five supra-tentorial abscesses requiring multiple neurosurgical procedures. No other cases have been identified in the literature which describe co-existent Nocardia and Enterococcus abscesses in an immunocompetent patient.
CASE REPORT
A 53-year-old male presented with a gradual onset of left-sided hemiplegia and weight loss of 14 kg over a period of ~4 weeks. His past medical history included COPD, hypertension and chronic hyponatraemia. There was no history of immunocompromise however he was malnourished. Of note, there was no history of foreign travel, intravenous drug use or household pets however the patient had undergone four dental fillings in the preceding 12 months. Neurological examination indicated MRC grade 2/5 power throughout the left upper and lower limbs with increased tone. The patient was apyrexic with a CRP of 68 mg/L.
A CT brain revealed a right frontal mass lesion with surrounding oedema which was concerning for malignancy when taken in conjunction with the weight loss. Investigations for a primary tumour were negative including a CT of the chest, abdomen and pelvis in addition to upper GI endoscopy. Tumour markers did not reveal any abnormality. Additional testing for immunocompromise including HIV was negative and no primary source of infection was identified. A subsequent MRI brain revealed a total of five ring-enhancing lesions with vasogenic oedema distributed throughout both cerebral hemispheres with the largest measuring >2 cm (Fig. 1).
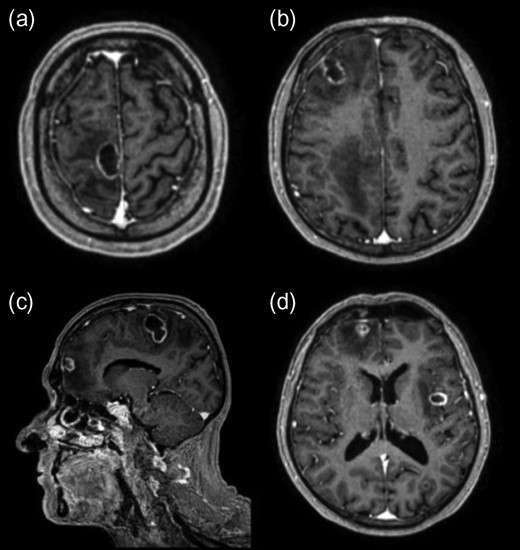
Initial post-contrast T1-weighted MRI demonstrating three lesions involving the right frontal lobe (a, b, c) with another in the left lateral occipital lobe (d) and one in the left insular region (d). The lesions also displayed complex walls typical of an abscess capsule on T2-weighted imaging and demonstrated central diffusion restriction (not shown).
Commencement of dexamethasone (8 mg twice-daily) initially resulted in a good clinical response. Image-guided excision of the right frontal abscess was undertaken and culture results identified Nocardia farcinica. Despite appropriate treatment with intravenous linezolid combined with imipenem and the subsequent addition of co-trimoxazole, repeat imaging demonstrated a continued increase in size of the remaining abscesses. Two further operations were performed over a 4-week period in addition to ongoing anti-microbial therapy. Resection of all abscesses was achieved through right frontal, right parietal, left parieto-occipital and left temporal craniotomies. Microbiological analysis identified Enterococcus faecium in a second abscess and vancomycin was added to the antibiotic regimen. Post-operative imaging indicated complete resection and appearances were monitored with regular imaging (Fig. 2). A prolonged course of dexamethasone was required to maintain neurological function. This may have contributed to a wound dehiscence requiring an uneventful wash-out and repeat closure in theatre. Ongoing seizure activity was controlled with anticonvulsants.
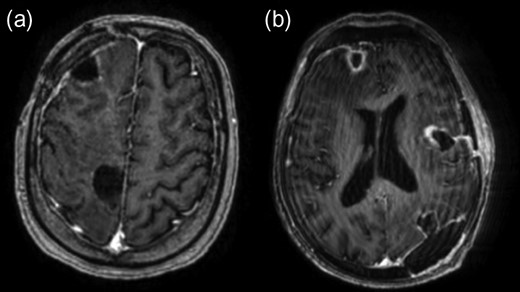
Post-contrast axial T1-weighted MRI following resection of abscesses in the right frontal lobe (a, b), left insular region (b) and left occipital lobe (b).
Due to fluctuating symptoms, the patient remained in hospital for the duration of intravenous antibiotics over a 4-month period. Oral ciprofloxacin (750 mg twice-daily) was commenced for one year on discharge in addition to a 2-week course of oral Linezolid (600 mg twice-daily). Despite early post-operative expressive dysphasia and slow resolution of left-sided weakness, there were no neurological deficits noted on discharge. Following in-patient rehabilitation, the patient was discharged to his own home. A follow-up MRI at 6 months from discharge has shown no evidence of disease recurrence.
DISCUSSION
Nocardia is a Gram-positive, aerobic, Actinomycete bacteria found in soil which is acquired primarily by inhalation with subsequent haematogenous spread. It is a particularly challenging infection to diagnose and treat as it may sometimes appear Gram-negative while prolonged culture time may result in masking by faster-growing, non-pathological organisms. Furthermore, resistance to empirical anti-microbial therapy for cerebral abscess including cephalosporins is common. Nocardia asteroides has previously been recognized as the most common Nocardia species causing brain abscesses in a large case series [1]. However, more recent case reports suggest N. farcinica is increasingly identified in this setting [3]. Unlike the case described in this report, these often relate to immunocompromised individuals. Enterococcus species are Gram-positive cocci and the majority of reported intracranial abscesses involve E. avium rather than E. faecium. Clinical outcomes are more favourable when compared to those with Nocardia abscesses [2]. A case of co-existing intracranial infection has not previously been reported.
The multiplicity of the abscesses, bilateral cerebral hemisphere involvement and absence of an identifiable site of primary infection are interesting aspects of this case which differ from previously reported cases of N. farcinica in the literature. These features also posed a challenge for surgical management. It has been demonstrated that patients with multiple Nocardia abscesses have an observed mortality of 66% in comparison to 33% for those with a single abscess [1]. This suggests that early recognition of lesions with prompt identification of the underlying organism is of particular importance in this subgroup to facilitate early surgical intervention and anti-microbial therapy tailored to sensitivities. Furthermore, progression of abscess formation despite anti-microbial therapy should prompt consideration of a second, co-existing microbial aetiology. The approach undertaken here to achieve a good outcome with no morbidity supports previously published recommendations endorsing aspiration of large abscesses with subsequent surgical excision if continued growth occurs following 2 weeks of antibiotic therapy [1].
In conclusion, this case report describes the successful treatment of multiple intracranial abscesses of dual anti-microbial pathology with surgical excision and appropriate anti-microbial therapy to achieve a good functional outcome. It adds to the available literature regarding the management of Nocardia cerebral abscesses and is the first description of co-existing intracranial E. faecium infection. This will be of importance in assisting recognition of this rare condition and to inform treatment strategies.
CONFLICT OF INTEREST STATEMENT
None declared.



