-
PDF
- Split View
-
Views
-
Cite
Cite
Yohei Kawatani, Yoshitsugu Nakamura, Takaki Hori, A case of chronic left main trunk occlusion treated with off-pump coronary artery bypass grafting, Journal of Surgical Case Reports, Volume 2018, Issue 2, February 2018, rjy006, https://doi.org/10.1093/jscr/rjy006
Close - Share Icon Share
Abstract
Ischemic heart disease presents with various symptoms, and chest pain is a chief complaint. Occlusion of the left main trunk often results in serious symptoms such as cardiogenic shock. However, while extremely rare, left main trunk occlusion can present with only slight chronic symptoms. In the present case, a 62-year-old woman with few risk factors for ischemic heart disease visited our hospital complaining of exertional chest pain, which had gradually intensified over the past several years. Coronary artery computed tomography revealed total occlusion of the left main trunk, which was examined closely using coronary angiography. Coronary angiography showed that the left coronary artery was perfused by collateral pathways from the right coronary artery. The patient was thus diagnosed with chronic occlusion of the left main trunk. She underwent off-pump coronary artery bypass grafting, which proved to be an effective treatment.
INTRODUCTION
In many cases of ischemic heart disease, patients arrive at a hospital with serious symptoms. However, this is not always the case, as total occlusion can develop acutely or chronically [1]. In an acute occlusion of the left main trunk (LMT), a large area of the myocardium becomes ischemic, often resulting in serious symptoms. In contrast, chronic total occlusion (CTO) has an asymptomatic period, and when diagnosed its symptoms are often slight. CTO of the LMT is an extremely rare pathology, observed in only 0.025–0.4% of patients who undergo coronary angiography [2].
CASE REPORT
A 62-year-old woman presented with exertional chest pain. She visited our hospital because her symptoms were gradually intensifying for several years. Her only risk factor for heart disease was hypertension; she had no history of smoking, and she did not have dyslipidemia. Electrocardiography did not show any ischemic changes. On echocardiography, left ventricular function was preserved and neither hypokinesia nor valvular heart disease was observed. Further evaluation of coronary artery disease was considered necessary; therefore, she underwent a detailed examination using coronary computed tomography (CT) (Fig. 1), which revealed an LMT occlusion. Coronary angiography also revealed that the LMT was occluded at the origin. The entire left coronary artery was visualized through collateral circulation in right coronary angiography (Fig. 2). Based on blood test findings and aortic CT results, arteritis and autoimmune disease were ruled out.
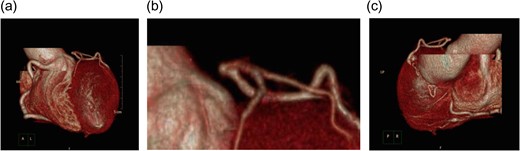
Coronary angiography at the time of the initial diagnosis. (a and b) Anterior-left lateral image and (c) posterior-right lateral view. The disruption of blood flow to the LMT can be seen. Despite this disruption, the left anterior descending coronary artery and the circumflex artery demonstrate contrast enhancement. There is no indication of calcification or other lesions in the LMT.
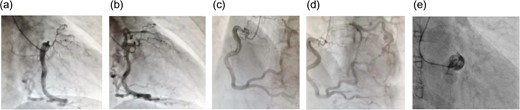
(a and b) Right coronary angiography: right anterior oblique projection; (c and d) right coronary angiography: left anterior oblique projection; (e) left coronary angiography. During left coronary angiography, only the sinus of Valsalva is visualized, and there is no antegrade contrast enhancement in the left coronary artery. The left coronary artery is visualized through collateral pathways from the right coronary artery. The right coronary artery is more developed than the left coronary artery, and several collateral pathways can be observed.
We performed off-pump CABG to treat this patient. We anastomosed the left internal thoracic artery to the left anterior descending coronary artery and the right internal thoracic artery to the left marginal artery. The patient’s hemodynamics were stable during and after the operation. The patient’s postoperative progress was smooth; her ventilator was removed the day after the operation, she began walking independently on Day 3 post-operation, and she was discharged on Day 8 post-operation. Graft patency was confirmed with coronary CT on Day 7 post-operation (Fig. 3). She goes well without any symptoms during 3-years follow up.
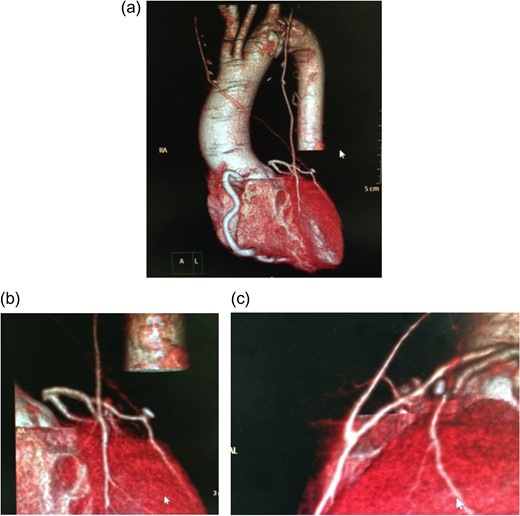
Postoperative coronary angiography. Complete graft patency was confirmed.
DISCUSSION
Coronary total occlusion can develop either acutely or chronically. When total occlusion develops acutely, it manifests as an acute myocardial infarction and often presents with ST elevation and other ischemic changes on electrocardiography. Depending on the site of the occlusion, it may also trigger a decline in left ventricular function. When acute total occlusion occurs in the LMT, a large area of the myocardium becomes ischemic; this can easily be a serious condition.
Chronic occlusion, on the other hand, is asymptomatic for 3 months or more and is sometimes asymptomatic when diagnosed [1]. Even when symptoms manifest, they often progress slowly. This is due to the blood flow from collateral pathways to the perfused portion of the occluded coronary artery.
This type of chronic occlusion in the LMT is rare, occurring in only 0.025–0.4% of ischemic heart disease patients [2]. In our hospital, from April 2014 to March 2015, coronary angiography was performed 3 841 times at our hospital for patients suspected of having ischemic heart disease. During this period, we observed only one case of LMT-CTO, which is approximately equivalent to its reported frequency.
In addition, the majority of patients (70–80%) who present with LMT-CTO have multiple lesions, whereas solitary LMT-CTO (such as the present case) accounts for only 6–9% of cases [2].
In the present case, no evident systemic disease such as arteritis or autoimmune disease was observed. There was no sign of iatrogenic causes, including complications of percutaneous coronary intervention (PCI). In addition, while the right coronary artery and collateral pathways from the right coronary artery to the left coronary artery were somewhat developed, these were not large enough to indicate that the LMT occlusion resulted from a congenital coronary artery anomaly. We believe that the LMT was occluded after birth and that collateral pathways developed as a result.
In LMT-CTO, antegrade blood flow in the LMT is not observed with left coronary angiography. Instead, a characteristic finding is observed, in which the left coronary artery is perfused from a collateral pathway developed from the right coronary artery [3].
As CTO gradually progresses, collateral pathways develop from the right coronary artery, resulting in the maintenance of blood flow to the myocardium in the perfusion region of the left coronary artery.
Coronary CT is also useful for diagnosis of occlusion of coronary artery [4]. Coronary CT enabled us to make a diagnosis of LMT-CTO and to make plans of surgery. Furthermore, aortic CT can be performed simultaneously with coronary CT, thus enabling simultaneous screening for aortitis and other systemic vascular diseases.
The success rate of PCI for CTO is reported to be 40–81%. When performing PCI for the LMT, the rate of restenosis when using a bare metal stent is 20%. Even when using a drug-eluting stent, the restenosis rate is still high, at 10% [5]. The 1-year mortality rate following the use of a bare metal stent is reported to be 3–28%, which represents a poor outcome [6].
Yip et al. [7] reported the results of PCI for total occlusion of the LMT in 8 patients and subtotal occlusion of the LMT in 10 patients. The procedural success rate in these cases was 72.2%. Of the 18 patients, 4 underwent re-treatment with CABG, 6 died in the hospital and 2 died after being discharged [4].
In a study in which 1800 patients with LMT lesions were randomly assigned to treatment with CABG or PCI using a drug-eluted stent, Morice et al. reported no significant difference in overall mortality. However, revascularization rate over a 5-year observation period was 21.6% for PCI and 15.5% for CABG; therefore, CABG was significantly superior [8].
In a study of the operative procedures during CABG for LMT lesions, Fukushima et al. compared on-pump (conventional coronary artery bypass; CCAB) and off-pump (off-pump coronary artery bypass; OPCAB) CABG in a group of subjects narrowed down from 257 consecutive patients after excluding patients who presented with cardiogenic shock. The overall graft patency rate was 97% with CCAB and 97.6% with OPCAB; thus, there was no significant difference between groups. Although there was no significant difference in mortality, OPCAB was superior to CCAB in terms of postoperative respiratory complications (CCAB: 3.1%, OPCAB: 2.5%), operative time, intraoperative blood loss and the number of cases in which transfusions were performed [9]. When hemodynamics are stabilized, as in the present case, off-pump CABG is the optimal operative procedure.
ACKNOWLEDGEMENTS
This case was presented in The 166th Meeting of The Kanto Koshinetsu area in The Japanese Association for Thoracic Surgery.
CONFLICT OF INTEREST STATEMENT
None declared.
CONSENT FOR PUBLICATION
Consent to publish was obtained in all cases from patients themselves or proxies with permission to make decisions on behalf of patients.



