-
PDF
- Split View
-
Views
-
Cite
Cite
Ajogwu U Ugwu, Naomi Kerins, Momin Malik, Traumatic small bowel perforation in a case of a perineal hernia, Journal of Surgical Case Reports, Volume 2018, Issue 12, December 2018, rjy330, https://doi.org/10.1093/jscr/rjy330
Close - Share Icon Share
Abstract
Perineal hernias following pelvic surgery are rare. Traumatic small bowel perforation in a patient with a perineal hernia is yet to be described. This case report describes a 69-year-old female who following an abdominoperineal resection for cancer developed a perineal hernia and unfortunately sustained perineal trauma. She presented with peritonitis and findings on laparotomy were that of two points of perforation to terminal ileal loop adherent to perineal defect. Resection and a side-to-side anastomosis performed. Repair of the hernia using mesh was considered but not performed due to risk of mesh infection. Perineal hernias have become more common since the advent of laparoscopic pelvic surgery. Although various methods have been described to repair these hernias, there is lack of robust evidence supporting one repair technique over others.
INTRODUCTION
A perineal hernia is an uncommon complication of major surgery involving the pelvis and its organs such as an abdominoperineal resection or pelvic exenteration. With such a rare phenomenon, the odds of traumatic bowel perforation are plausible but, somewhat mythical. We present such a ‘mythical’ case and we hope to highlight the need for increased vigilance and awareness in dealing with perineal hernias. Also, consideration should be given to the prevention and management of perineal hernias.
CASE REPORT
An elderly female presented to accident and emergency after a fall at home. She had been unwell for a couple of days and on the day of presentation felt dizzy and on the way to the bathroom fell landing on her perineum. She also describes some blunt head trauma on her way down, her head hitting the sink. She, however, denied any loss of consciousness.
Her background is significant for having had neoadjuvant chemotherapy and a laparoscopic AP resection for T2N0 rectal cancer in 2012. Her most recent surveillance CT in 2016 did not show any evidence of local recurrence, lymphadenopathy or distant metastasis. She had a perineal hernia which was being managed conservatively.
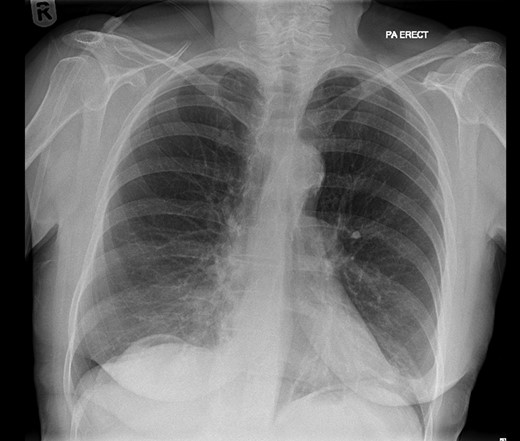
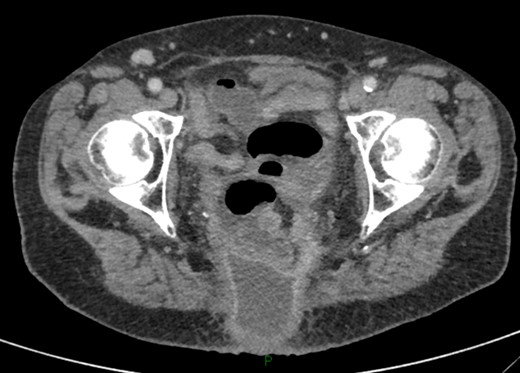
On examination, she was febrile. Her abdomen was generally tender. Bowel sounds were present and up to that time her stoma was working. Her perineal hernia was red and tender. Her initial CXR (Fig. 1) did reveal a sliver of gas underneath her right hemidiaphragm and in keeping with her abdominal findings she progressed to further imaging. CT abdomen pelvis with contrast showed pneumoperitoneum (Fig. 2) with ‘a tiny pocket of air is also seen adjacent to a loop of bowel in the pelvis posterior to the bladder’. ‘Exact site of perforation has not been demonstrated but could possibly be in the bowel loops in the perineum’ (Figs 3 and 4).
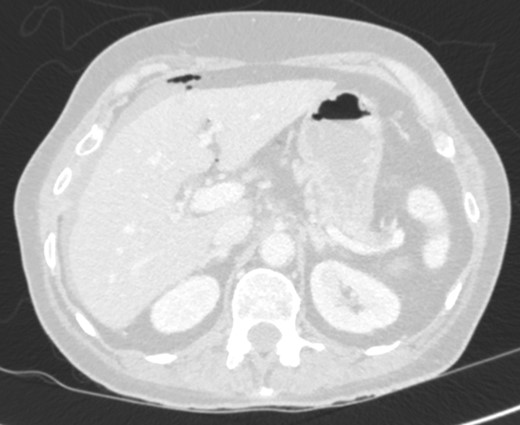

CT showing small bowel loops in pelvis with perineal hernia and free fluid.

Sagittal view showing small bowel loops in pelvis with perineal hernia.
She was resuscitated and had an emergency laparotomy which revealed a loop of terminal ileum herniating through the perineum with a band adhesion. The two sites of perforation (Fig. 5) with clean edges were seen in this terminal ileal loop, most likely caused by shearing due to the adhesion and hernia neck during the fall. These were resected, and a side-to-side anastomosis performed considering the limited peritoneal contamination. Repair of the hernia using mesh was considered but not performed due to the risk of mesh infection. There were no other injuries. She recovered well from her operation and went home on the eighth postoperative day with a plan for review at outpatient clinic to discuss repair of her hernia.

Loop of adherent small bowel stuck in perineal hernia with sites of perforation.
Unfortunately, she was readmitted after 5 weeks on account of being generally unwell, night sweats, CRP not improving at which time CT scan showed a fluid collection (Fig. 6) where the previous perineal hernia was, extending back to the skin surface posteriorly. Her condition was further complicated by a myocardial event which has now precluded any repair of her perineal hernia.
DISCUSSION
Perineal hernias are either primary or secondary and can be further classified into anterior and posterior by the transverse perineal muscle [1]. Perineal hernias are rare. Aboian et al. [2] in a retrospective study of 1266 patients post APR describe a complication rate of 0.39% and even less so in those post pelvic exenteration 0.15%. The possibility post proctocolectomy is even less with a rate of 0.09%. A retrospective review of patients with postoperative perineal hernia spanning 32 years describes a 0.62% complication rate post APR [3]. These are secondary perineal hernias. We now know risk factors include pre-operative radiotherapy, female gender and postoperative perineal wound infection [4].
No specific complications to a perineal hernia have been described in the literature. Here, we describe a traumatic bowel perforation following injury to the perineum in a person with a perineal hernia. A search of PubMed database with keywords, perineal hernia, trauma and bowel perforation had a negative yield.
Prior to the laparoscopic era, perineal hernias in human beings were almost unheard of. This may be attributed to the fact that at open procedure involving the pelvis, it was routine to reconstruct the pelvic peritoneum and this is a modality which has been left behind in the laparoscopic era. Several surgeons can attest to this, e.g. a senior surgeon with 20 years’ experience performing open APR with routine reconstruction of pelvic peritoneum describes no development of perineal hernia. However, since adoption of laparoscopic approach over 4 years there have been 2 out of 12 cases [4]. This would require further randomized controlled studies to prove, however, this would require a change in surgical practice.
Much has been documented on modalities for repair of a perineal hernia. Various approaches have been described namely laparoscopic, transabdominal, transperineal or combined approaches with various degrees of success. It is our suggestion that surgical practice should be modified with a view to prevention of this problem by reconstruction of the pelvic peritoneum after laparoscopic APR as is already being practiced during an open procedure. This has also been proposed by other colleagues [4].
It is envisaged that as laparoscopic APR and other pelvic procedures become more widespread and we do know that formation of adhesions is less in laparoscopic procedures, it is reasonable to expect perineal hernias to be become less rare and we would need to propose more efficient ways for repair and develop a gold standard for repair.
CONCLUSION
Perineal hernias have become more common since the advent of laparoscopic pelvic surgery. This may be due to the formation of fewer adhesions post-operatively, or because the pelvic peritoneum is not routinely closed in laparoscopic pelvic surgery. However, the evidence supporting these theories is observational at best and randomized controlled trials are recommended. Although various methods have been described to repair these hernias, there is lack of robust evidence supporting one repair technique over others.
ACKNOWLEDGEMENTS
A.U.U.: Identified the case, carried out the background research, wrote the draft and formatted the report. N.K.: Wrote the draft, reviewed the final draft. M.M.: Consultant surgeon who performed the operation. Oversaw the writing and editing of the report.
CONFLICT OF INTEREST STATEMENT
No conflict of interest.
ETHICAL APPROVAL
None required.
SOURCES OF FUNDING
No funding provided for this case report.



