-
PDF
- Split View
-
Views
-
Cite
Cite
Patrick Downs, Nicki Downes, Emily Zayshlyy, Christopher Esper, Pablo Giuseppucci, Internal hernia through the foramen of Winslow, Journal of Surgical Case Reports, Volume 2018, Issue 12, December 2018, rjy329, https://doi.org/10.1093/jscr/rjy329
Close - Share Icon Share
Abstract
Foramen of Winslow hernias are one of the most uncommon types of internal hernias that a surgeon will encounter. They are often initially indolent with vague symptoms that present over an extended period of time. Unfortunately, these hernias are not often diagnosed prior to requiring emergent operative intervention. This case report describes a patient who had a long history of vague abdominal pain and radiographic evidence of a foramen of Winslow hernia 4 years prior to presenting with acute obstructive symptoms. This raises the question: Should foramen of Winslow hernias, if diagnosed early, be repaired on an elective basis?
INTRODUCTION
Internal hernias have been defined as a passage of an organ through an intra-abdominal orifice, natural or pathologic. This could involve the omentum, the mesentery, or a peritoneal ligament. The foramen of Winslow is an anatomical opening that allows for just such a herniation. The onset of symptoms is frequently insidious and the clinical picture can range from nonspecific abdominal pain to the typical obstructive symptoms.
These patients will often be middle-aged adults who finally present with an acute surgical abdomen [1]. Imaging can play a vital role in diagnosis. On computed tomography (CT), visualizing loops of bowel between the liver and Inferior is highly suggestive for this type of hernia. Foramen of Winslow hernias account for 8% of internal hernias [1] and 0.08% of all hernias [2].
As with any internal hernia, treatment of foramen of Winslow hernias often requires expedient surgical intervention and possible resection of any necrotic bowel. Herniation of the small bowel accounts for 63% and the transverse colon for 7% of foramen of Winslow hernias [2]. This case report describes a patient who experienced just such a herniation involving both the transverse colon and small bowel.
CASE REPORT
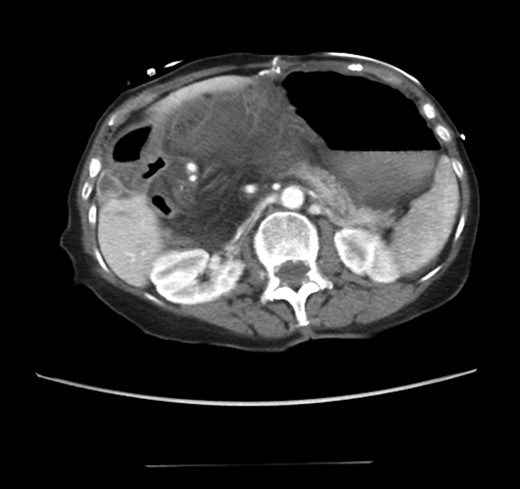
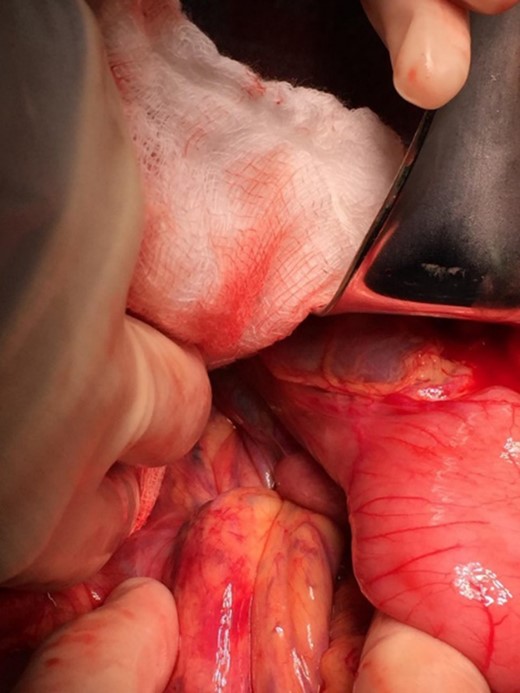
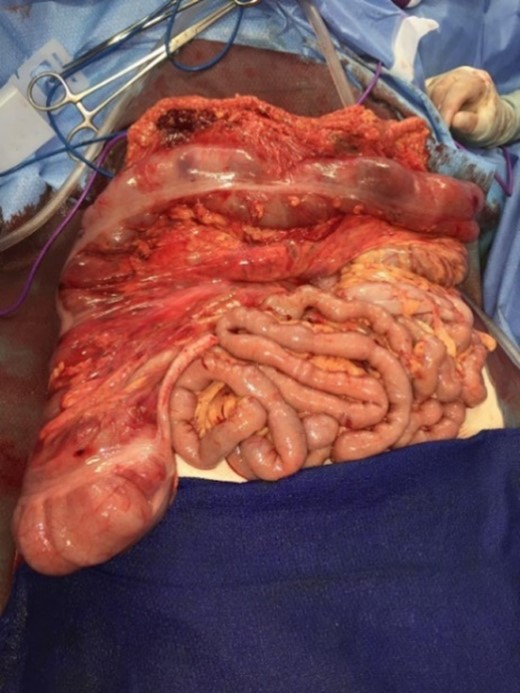
An 81-year-old female with a medical history of CAD with stents, hyperlipidemia, hypothyroidism, GERD, recent UTI, pancreatic cyst, constipation, anemia and leukopenia presented to the ED with a 1 day history of mild, diffuse and cramping abdominal pain. The patient was unable to give an accurate history, but the son at bedside supplemented this reporting that for several years the patient had been experiencing ill-defined abdominal discomfort. Physical exam showed a soft abdomen with mild tenderness and no evidence of peritonitis. A CT scan of the abdomen and pelvis with IV and PO contrast (Fig. 1) showed edematous changes to the mesentery of the small and large bowel with swirling of vessels indicative of internal hernia. The stomach was also noted to be distended with both air and fluid as a consequence of posterior compression by the hernia contents (Fig. 2). A surgical consult was obtained, a nasogastric tube and Foley catheter were placed, antibiotics were started, and the patient was taken for an exploratory laparotomy. Upon entering the abdomen through a vertical midline incision, 1.5 l of ascites was drained revealing a diffusely edematous mesentery. A large portion of the small bowel was seen to be herniated through the Foramen of Winslow (Fig. 3). A Kocher maneuver and division of the gastrocolic ligament were then performed to allow release of the herniated small bowel. It was at this time that, in addition to small bowel, a large portion of the ascending and transverse colon was noted to be herniated through the foramen of Winslow. The small bowel was also seen to be torsed about its own mesentery. Normal anatomy was restored and the bowel noted to be healthy and viable with peristalsis (Fig. 4). Due to the large size of the foramen after reduction and enlargement, it was deemed best to leave it open to prevent any further incarceration or strangulation. The abdomen was closed and the patient tolerated the procedure well. At a follow-up visit 2 months later, the patient had well-healed incisions, was doing well, tolerating a diet, and gaining weight appropriately.

Externalized abdominal contents shown to be pink and healthy bowel with some areas of ecchymosis in the transverse colon.
Loops of bowel between IVC, liver, and lesser curvature of the stomach. Arrow small bowel. Arrow head stomach.
CT scan from four years prior to presentation showing evidence of foramen of Winslow hernia. Arrow head on stomach. Arrow on bowel.
DISCUSSION
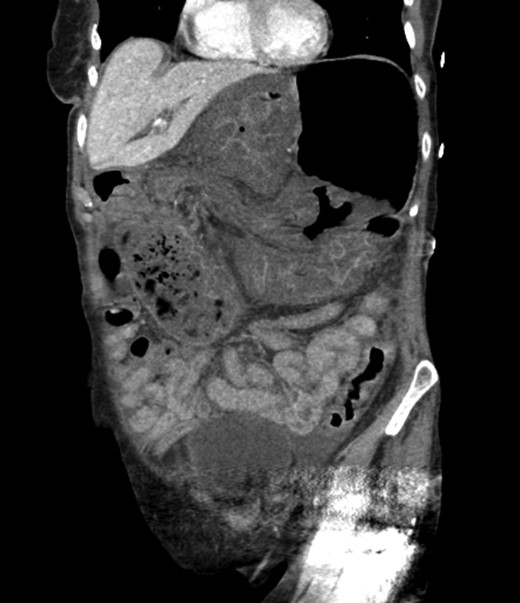
Diagnosing an internal hernia is frequently accomplished using physical exam and CT imaging. Abdominal X-ray does have some nonspecific findings suggestive of internal hernia but is usually inadequate for diagnosis. Diagnosis of a foramen of Winslow hernia, however, is only accomplished in 10% of patients preoperatively [3]. As previously mentioned this diagnosis is rare and often presents with vague obstructive type symptoms. This likely contributes to the low occurrence of accurate preoperative diagnosis. However, several radiographic findings were seen in this patient that suggested a foramen of Winslow hernia preoperatively. First, there is visible swirling of the mesentery on the CT scan that is indicative of internal hernia (Fig. 1). Second, there are loops of small bowel that can be visualized between the IVC and the edge of the liver in a supra renal position along the lesser curvature of the stomach (Figs 1 and 2). When compared to a CT of the abdomen and pelvis obtained 4 years prior to presentation, there is actually evidence that this patient had a non-obstructing foramen of Winslow hernia at that time as demonstrated by bowel being visualized in the lesser sack (Fig. 5). These findings, especially small bowel along the lesser curvature of the stomach, are inconsistent with normal anatomy and strongly indicative a foramen of Winslow hernia.
CT abdomen and pelvis coronal view of foramen of Winslow hernia.
The management of a foramen of Winslow hernia requires surgical reduction in the presence of obstructive symptoms with careful evaluation of the herniated bowel for non-reversible ischemia. This can be accomplished using laparoscopic techniques as described by Brandao et al. for small bowel [4], or using a laparotomy incision as in this case.
Laparoscopic reduction of the transverse colon from the foramen of Winslow has been successfully demonstrated when the hernia is easily reducible [5]. This case required laparotomy and enlargement of the foramen for reduction and prevention of future incarceration. Another approach is to cover the defect with omentum in hopes that as the body recovers, the omentum will adhere to the foramen and prevent future herniation.
In efforts to reduce the herniation, it may be necessary to decompress the herniated bowel and subsequently resect any ischemic portion. During a laparotomy, the bowel can be reduced by inserting the operator’s digits through the foramen for manual reduction [6]. Additionally, the foramen can be enlarged with a Kocher maneuver depending on the degree of herniation. Just such a maneuver was described in this case report. in conclusion, the fact that this patient had evidence of a non-obstructing foramen of Winslow hernia on CT scan 4 years prior to her presentation and surgical intervention raises the question, should these herniations be repaired operatively on an elective basis to avoid emergent surgery?
CONFLICT OF INTEREST STATEMENT
None declared.



