-
PDF
- Split View
-
Views
-
Cite
Cite
Ameen Barghi, Mark Wu, Viet Nguyen, Rebecca Osgood, Arundhati Ghosh, Minimally invasive drainage of a giant ovarian mucinous cystadenoma associated with a mature cystic teratoma, Journal of Surgical Case Reports, Volume 2018, Issue 11, November 2018, rjy322, https://doi.org/10.1093/jscr/rjy322
Close - Share Icon Share
Abstract
A 26-year-old, otherwise healthy female presented to the Emergency Room for the evaluation of abdominal pain. It was immediately apparent that she had a massively distended abdomen. History revealed progressive abdominal distension over several years. Evaluation for pregnancy was negative and a computed tomography (CT) scan demonstrated a 38 × 32 × 23 cm septated cystic mass. Careful controlled partial needle decompression of the cyst, removing 18.5 l of fluid, was followed by a mini-laparotomy with complete removal of a multi-loculated cystic ovarian mass approximately 45 lb in weight. Pathology was consistent with mucinous cystadenoma of the ovary in association with a mature cystic teratoma. This surgical technique of percutaneous drainage of the cyst, followed by mini-laparotomy is a valuable example of a safe and effective minimally invasive treatment modality for giant ovarian mucinous cystadenomas.
INTRODUCTION
Ovarian mucinous cystadenomas are benign tumors that arise from ovarian epithelium. They primarily occur in the 30s and 40s, rarely before puberty or after menopause [1]. They are extremely rare in developed countries such as the United States. Cysts greater than 10 cm in size are classified as ‘giant’ ovarian mucinous cystadenoma (GOMC). They are large, smooth, loculated and filled with glycoprotein-rich fluid. GOMCs may adhere to nearby organs causing symptoms. Mucinous tumors comprise 15% of ovarian tumors, with 80% being benign [2]. While GOMCs are exceedingly rare as a single entity, association with another ovarian tumor is even rarer. We report the case of a GOMC that is not only one of the largest reported in the literature but also in association with a mature cystic teratoma. To our knowledge, no previous report of coexistence of these two tumors has been reported and treated via a safe and effective minimally invasive treatment modality for these giant tumors.
CASE REPORT
A 26-year old female with a 4-year history of progressive abdominal swelling with no other past medical or surgical history presented to the emergency room complaining of increasing periumbilical pain for 2 days. The patient denied any associated symptoms such as fever, chills, nausea, emesis, dyspnea, diarrhea, constipation, dysuria or vaginal bleeding but did endorse a 30-pound weight loss over 6 months.
The patient was 168 cm tall and weighed 194 lb (88 kg). On physical exam, the most notable finding was a massively distended abdomen consistent in size with a 9-month gestation. The patient appeared cachectic, with stable vital signs and in no acute distress. Abdomen was non-tender, with prominent veins on the lateral aspects and an easily elicited fluid wave. Urine pregnancy test was negative; bedside ultrasound did not demonstrate an intrauterine pregnancy, but did show a massive fluid-filled mass. Laboratory evaluations, including tumor markers (CA19-9, CA 125, CEA and AFP), were all within normal limits. A CT scan (Fig. 1A and B) demonstrated a large 38 × 32 × 23 cm cystic collection occupying most of the abdominal and pelvic cavity with multiple thin septations but no discrete soft tissue mass or mural nodules. All of the abdominal organs were displaced by the cystic collection. No other pathology was identified.
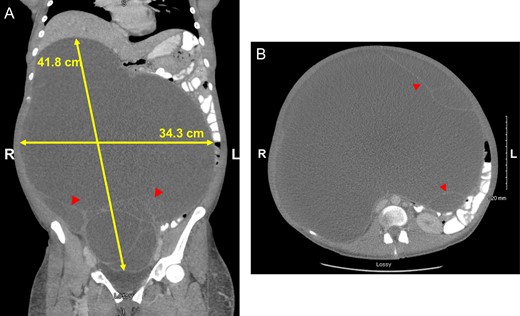
Coronal (A) and axial (B) views highlighting size of GOMC, displacement of abdominal organs and cystic loculations (arrowheads).
After careful multidisciplinary planning, the patient proceeded to the operating room (Fig. 2A). General anesthesia was administered; a careful percutaneous decompression was first performed with an 18-gauge needle. During decompression, hemodynamics were carefully monitored. After removing 8 L of fluid from the cyst, the abdominal cavity was accessed via a 2.5-cm infraumbilical midline incision. A purse-string suture was placed on the cyst wall and an opening was made into the cyst, with further cyst decompression by direct suction. Once the dominant loculation was completely aspirated, the purse-string suture was closed. The other loculations were similarly decompressed in a controlled fashion. A total of 18.5 l of serous, dark, blood-tinged fluid was aspirated. The cyst wall was then sequentially pulled out through the abdominal wall opening. The entire mass, weighing 45 lb (Fig. 2B) was exteriorized out of the abdomen. At this point, it was evident the giant mass was arising from the right ovary, while the uterus, left fallopian tube, and left ovary were normal. The gynecology team completed a right salpino-oophorectomy.

Patient supine prior to percutaneous drainage (A) and whitish cyst wall after drainage (B).
Pathology demonstrated a mucinous cystadenoma with focal proliferation arising in association with a mature cystic teratoma. The two tumors were distinct and no transitional features were recognized histologically. Many of the locules were lined by a single layer of cuboidal to columnar mucinous epithelium with occasional macrophages containing hemosiderin. Focal areas showed proliferation, representing less than 10% of the cyst lining (Fig. 3).
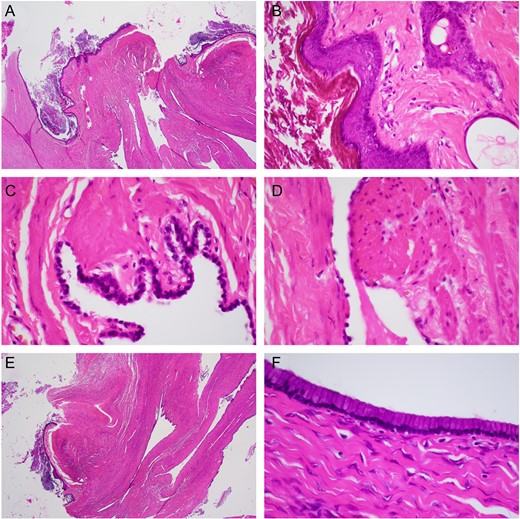
(A) Low power (20×) of mature cystic teratoma lined by ectodermal squamous epithelium (arrowhead), cutaneous appendages, and endodermal glandular/gastrointestinal epithelium. (B) High power (400×) mature cystic teratoma lined by ectodermal squamous epithelium cutaneous appendage (arrowhead). (C) High power (600×) ciliated endodermal respiratory epithelium (arrowhead). (D) High power (600×) endodermal smooth muscle (arrowhead). (E) Low power (20×) mucinous cystic teratoma with adjacent mucinous cystadenoma (arrowhead). (F) High power (400×) mucinous cystadenoma.
The patient’s post-operative course was uncomplicated and she now weighed 149 lb (67.6 kg).
DISCUSSION
Giant ovarian tumors are a known entity, but very rare in developed countries given that most ovarian masses are discovered early on routine medical visits. Most reported cases are from developing regions such as India [3] or Africa [4]. Mucinous cystadenomas are typically unilateral, benign tumors of epithelial origin lined by tall columnar, non-ciliated epithelial cells with apical mucin and basal nuclei. In a 20-year retrospective study of ovarian teratoma, Caruso et al. document 305 cases of ovarian teratoma, of which only 4 were found in association with mucinous cystadenoma. All four were < 15 cm in size [5]. Upon extensive review of the literature, we believe this report is the first case study of giant mucinous cystadenoma arising alongside ovarian teratoma.
GOMCs may have several clinical manifestations including orthopnea/dyspnea, difficulty ambulating, tachycardia, abdominal compartment syndrome [6], inferior vena cava compression and subsequent lower extremity edema, and respiratory manifestations such as atelectasis and pulmonary edema [7]. Our patient’s presentation of abdominal pain and cachexia was likely secondary to early satiety caused by the tumor’s mass effect. Malignancy rates up to 37% have been reported for giant ovarian cysts [8]. Malignant transformations of the cystic teratoma component is even smaller at 1–3% [9]. Recurrence is rare with complete excision and oophorectomy.
There is no consensus on whether laparoscopy or laparotomy should be used in the case of benign giant ovarian cysts [8]. To avoid the previously studied decompression syndrome [8], we initially performed a slow, controlled percutaneous decompression using a large bore needle connected to a 3-way stopcock. This collapsed the cyst to a more manageable size, allowing the removal of the giant mass through a very small incision, without any spillage of contents. We chose an open surgery through a small infraumbilical midline incision, following controlled decompression of the cyst.
We present one of the largest tumors and the only case report to date of GOMC arising from ovarian teratoma. Most GOMCs respond well to surgical removal, though a standardized approach has yet to be established. This surgical technique of percutaneous drainage of the cyst, followed by mini-laparotomy is a valuable example of a safe and effective minimally invasive treatment modality for giant ovarian mucinous cystadenomas.
CONFLICT OF INTEREST STATEMENT
None Declared



