-
PDF
- Split View
-
Views
-
Cite
Cite
Vinu Perinjelil, Kwabena Nkansah-Amankra, Tareq Maraqa, Leo Mercer, Gul Sachwani-Daswani, Endo GIA stapler malfunction in a small bowel loop resection, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy281, https://doi.org/10.1093/jscr/rjy281
Close - Share Icon Share
Abstract
Endovascular gastrointestinal anastomosis (Endo-GIA) staplers are widely used in various surgical procedures despite difficulties in operating them and associated mechanical failures. We present a case of a patient whose post-operative recovery was complicated by intraoperative Endo-GIA stapler failure, which is rarely reported in literature. Our report describes the behavior and consequences of surgical stapler failure so surgeons can anticipate challenges of newer surgical devices while maintaining optimal patient outcomes.
INTRODUCTION
Endovascular gastrointestinal anastomosis (Endo-GIA) staplers are effective alternatives to suturing in surgery. They offer a faster way to divide and join the bowel and are easier to master in comparison to laparoscopic hand suturing [1]. Powered laparoscopic staplers result in shorter operating times and lower infection rates. However, complications can arise, which include leakage from staple lines, fistula formation and bleeding [2]. Though rare, there have been reports of malfunctioning of GIA stapler in laparoscopic procedures resulting in conversion to an open procedure. Despite this, there is a scarcity of information on malfunctioning Endo-GIA staplers. We report a case of stapler failure in a small bowel resection to add to the literature.
CASE REPORT
A 72-year-old man with past medical history including hypertension, chronic kidney disease, cerebrovascular disease and chronic obstructive pulmonary disease presented to the emergency department with altered mental status and abdominal pain. Physical exam revealed non-radiating pain localized to the right lower quadrant absent of alleviating or exacerbating factors and without associated symptoms. Computed tomography (CT) Imaging was concerning for ruptured appendicitis and clinical exam was consistent with peritonitis and sepsis. Patient was promptly taken to the operating room for an exploratory laparotomy, ileocecotomy, appendectomy, drainage of abscess and ileostomy. Patient was prepared and positioned for surgery in supine position. During the procedure, mild hyperemia of the appendix was noted. Approximately 7 cm proximal to the ileocecal valve, the terminal ileum was transected using a 55 mm GIA blue load. The proximal part of the cecum was freed from peritoneal attachment. The cecum was transected using a 75 mm GIA blue load. All the mesentery between the two transected points was taken down using the ligature. A few days later, dehiscence of the staple line on the ascending colon occurred. The patient was taken back to the operating room for exploratory laparotomy and repair of the dehiscence. Midway through, another attempt to transect the proximal part of ascending colon using powered Endo-GIA stapler failed (Fig. 1). The stapler abruptly froze; a sound went off and it became locked. Repeated attempts to override using the manual handle failed and it took over 10 min to separate the stapler sides. A contour stapler was then used instead of the powered stapler for segmental transection of the ascending colon. His hospital course was complicated by recurrent ileostomy necrosis and futile wound healing, resulting in colonic suture breakdown with recurrent fecal peritonitis and septic shock, acute renal failure requiring dialysis, acute respiratory failure requiring trach and right upper extremity deep venous thrombosis. The patient required delayed abdominal wound closure due to recurring intra-abdominal sepsis. His post-operative management was complicated by high ileostomy output which did not readily slow with multiple modalities to control gastrointestinal loss. Patient required on-going resuscitative hydration with IV fluid boluses to compensate for his high output ileostomy. Patient was discharged after 8 weeks in fair condition to a nursing care facility.
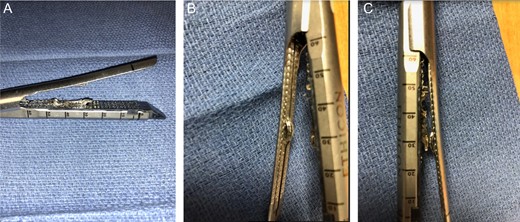
(A–C) Powered Endo-GIA stapler after intraoperative mechanical damage.
DISCUSSION
In this report, we describe the malfunctioning of an Endo-GIA stapler in a large bowel resection. Surgical staplers have been in widespread usage since the 1970s. Intestinal staplers work by bringing the edges of wounds together along with blood vessels; essentially acting as a hemostat and sealer to the area [3]. There are two forms currently in use: ‘B’ and relatively newer ‘D’. The ‘B’ shape allows for high delivery profile, whereas the ‘D’ shape relies on a low-profile of the applicator. To be considered effective, a staple line must allow adequate tissue perfusion while minimizing bleeding and tissue destruction [4]. To enable this, factors such as tissue thickness, type, compression and staple height must be taken into consideration. Being able to maximize tissue-stapler interaction accelerates the wound healing process. Research has shown that when all aforementioned variables are kept equal, the ultimate determinant is surgeon experience [4]. A retrospective review of the United States Food & Drug Administration (FDA)-Manufacturer and User Facility Device Experience (MAUDE) looking at staple malfunctioning during laparoscopic nephrectomy reported that out of 502 documented failures, there were a host of underlying reasons [5]. A total of 60% was due to a leaking staple line after firing and 10.8% was due to a locked stapler with inability to release from tissue. Hemorrhage with >500 ml blood loss was reported in 42.5% of cases in this study. Additionally, five deaths were attributed directly to device failure [5]. While newer mechanical devices are introduced with modifications to improve the safety profile, each stapler has the potential to fail given enough use and familiarity with technical details can avoid adverse events. Unlike others, our case report reports an instance of mechanical failure which resolved intraoperatively without prolonged delay or post-operative complications related to malfunction. Furthermore, this case emphasizes the importance in preparing surgeons to address technical issues that arise intraoperatively to avert post-surgical complications.
CONCLUSION
Endo-GIA staplers, though useful, can have severe consequences in the event of malfunctioning with potential to adversely affect patient outcome. Surgeons cognizant of this possibility will be prepared to salvage a malfunctioning stapler with suitable approaches. Educational programs that keep surgeons informed of optimal techniques to employ and common problems to troubleshoot should be a priority [6]. In the future, retrospective cohort studies or a prospective randomized control trial assessing stapler failure should be conducted.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
Hurley Medical Center.



