-
PDF
- Split View
-
Views
-
Cite
Cite
Luke Traeger, George Kiroff, Intrabilary obstruction by colorectal metastases, Journal of Surgical Case Reports, Volume 2018, Issue 1, January 2018, rjx259, https://doi.org/10.1093/jscr/rjx259
Close - Share Icon Share
Abstract
Intrabiliary colorectal metastases are rare. We present a case of an 84-year-old man who developed obstructive jaundice secondary to intrabiliary growth of colorectal metastases. The patient presented with three weeks of jaundice and significant weight loss in the preceding months. The patient’s background included metastatic colorectal carcinoma, with a previous right hemicolectomy and left hepatectomy for liver metastases. A MRCP showed an obstruction of the biliary tract transitioning at the ampulla. Histology confirmed a malignant adenocarcinoma. When compared to the patient’s previous resected colorectal liver metastases, morphology and immunohistochemistry was consistent with colorectal metastases. This case highlights the importance of differentiating a new intraductal papillary neoplasm from a colorectal metastasis. Correctly identifying these lesions requires the use of MRCP and ERCP, as well as immunohistochemistry. This is a priority for clinicians to ensure appropriate therapy.
INTRODUCTION
Intrabiliary colorectal metastases are rare, representing 4.5% of all colorectal hepatobiliary metastases [1]. Only half of these metastases will have evidence of a biliary dilation or obstruction [1]. Differentiating a new intraductal papillary neoplasm from a colorectal metastasis is difficult, relying on immunohistochemistry.
CASE REPORT
An 84-year-old man presented to the Emergency Department with a 3-week history of jaundice. He reported recent dark urine and weight loss of 8 kg over the preceding 3 months. The patient had a previous history of metastatic colorectal carcinoma, with a right hemicolectomy four years ago and a left hepatectomy one year ago for liver metastases. Bloods revealed a bilirubin of 224 U/L and raised liver enzymes consistent with an obstructive picture. He was admitted to the hospital and underwent a magnetic resonance cholangiopancreatography (MRCP). MRCP (Fig. 1) showed obstruction of the biliary tract transitioning at the ampulla. An endoscopic retrograde cholangiopancreatography (ERCP) demonstrated no choledocholithiasis; however, showed a likely malignant stricture. A sphincterotomy was performed, the common bile duct was dilated, and a biopsy and bile duct brushings were taken. As the patient was a poor surgical candidate, a metallic stent was inserted. Histology of the bile duct biopsy showed intestinal differentiation and was morphologically similar when compared to the patient’s previous resected colorectal liver metastases. Bile duct brushings showed malignant cells consistent with adenocarcinoma. Immunohistochemistry was cytokeratin-7(CK-7) negative and CK-20 positive, favouring an intrabiliary colorectal metastasis over a new primary bile duct carcinoma. Post-metallic stent insertion, the patient had a resolution of his elevated bilirubin and was referred to Medical Oncology for palliative chemotherapy.
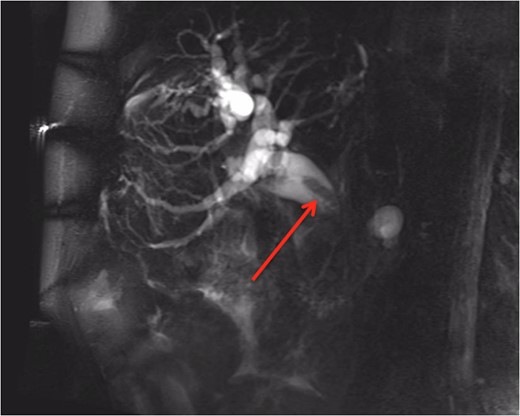
MRCP showing an obstruction of the biliary tract (identified with red arrow) transitioning at the ampulla.
DISCUSSION
Approximately 93% of all intrabiliary metastases have been shown to be of colorectal origin, with lung and kidney accounting for the majority of the remainder [1, 2]. In all, 50% of intrabiliary colorectal metastases are found in major bile ducts [2, 3]. Intrabiliary colorectal metastases are generally identified within 28 months of resection of the primary tumour [4].
In our case, jaundice was the prominent feature leading to diagnosis. Jaundice and increasing carcinoembryonic antigen (CEA) are the most frequent clinical signs raising the suspicion of intrabiliary colorectal metastases, however, these signs do not allow differentiation from alternative diagnosis [5]. Computerized tomography (CT), which is commonly used for monitoring of colorectal cancer, does not reliably make a diagnosis of intrabiliary colorectal metastases [6]. CT changes can be subtle and dilation of ducts may be the only identifiable abnormality [6]. MRCP is preferred imaging modality if intrabiliary metastasis is suspected.
Differentiating an intraductal papillary neoplasm from colorectal metastases relies heavily on immunohistochemistry. Primary biliary and pancreatic adenocarcinomas are CK-7 positive in 71–100% of cases and CK-20 positive in 22–46% of cases [7]. Colorectal metastases are CK20 positive in 91–100% of cases and are uncommonly CK-7 positive [7]. Thus in our case the intrabiliary lesion is most consistent with a colorectal metastases. Differentiating between intraductal papillary neoplasm and colorectal metastases should be a priority for clinicians to ensure appropriate therapy [8]. Incorrectly identifying intrabiliary colorectal metastases as an intraductal papillary neoplasm can lead to more radical resection as opposed to a limited resection [5].
Ideal treatment of patients with colorectal metastasis and macroscopic intrabiliary growth requires an anatomical hepatobiliary resection [5]. Failure to identify intrabiliary invasion when performing resection for liver metastasis leads to unexpected recurrences [1]. If surgical resection is not considered appropriate, as with our case, the use of metal stent is preferable. Metal stenting with ERCP has been shown to reduce rate of occlusion, lower stent failure rates and less frequent episodes of cholangitis compared to plastic stenting [7].
In summary, intrabiliary colorectal metastases are a rare finding. Patients presenting with jaundice and a past history of colorectal cancer should be approached with a high level of suspicion for intrabiliary metastases. MRCP and ERCP are considered integral in identifying intrabiliary lesions. Clinicians should be aware that correctly identifying intrabiliary lesions is important, as incorrect therapy can be harmful to patients.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- immunohistochemistry
- weight reduction
- adenocarcinoma
- endoscopic retrograde cholangiopancreatography
- biliary tract
- jaundice
- neoplasm metastasis
- histology
- neoplasms
- liver metastases
- magnetic resonance cholangiopancreatography
- jaundice, obstructive
- colectomy, right
- colorectal cancer metastatic
- hepatectomy, total left lobectomy



