-
PDF
- Split View
-
Views
-
Cite
Cite
Marson Davidson, Miriam Aioub, Martin Gutierrez, Kunchang Song, Ellen Hagopian, Martin Karpeh, Operable synchronous ampullary carcinoma and hepatocellular carcinoma: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2017, Issue 9, September 2017, rjx182, https://doi.org/10.1093/jscr/rjx182
Close - Share Icon Share
Abstract
We report a rare case of synchronous double primary malignancies of the liver and ampulla. A 70-year-old white female was diagnosed with ampullary and hepatocellular carcinoma. The management and outcome of this rare case of synchronous double primary hepatic and periampullary malignancies, amenable to surgical resection is discussed.
INTRODUCTION
Hepatocelllar carcinoma (HCC) is the third leading cause of cancer related death worldwide with an annual incidence of at least 6 per 100 000 in 2010. The number of deaths per year due to HCC is virtually identical to the worldwide incidence, delineating the lethality of this disease [1]. Ampullary adenocarcinomas are rare and account for 0.5% of gastrointestinal malignancies [2]. The etiology of ampullary cancers is unknown. Only one case of synchronous HCC and pancreatic cancer has been reported in the literature [3]. Furthermore, there are no reports of resected synchronous HCC and periampullary carcinomas. We herein report the first case of simultaneous resection of synchronous hepatocellular and ampullary carcinomas.
CASE REPORT
A 70-year-old woman presented with right-sided abdominal pain, nausea, vomiting and fever. She had a history of diabetes, hypertension and hypercholesterolemia. She smoked 0.5 pack/day and denied alcohol abuse. There was no significant family history. On admission her vital signs were within normal limits. On physical exam her sclera were anicteric. Her abdomen was soft, non-tender, non-distended with no palpable masses. Labarotory studies revealed: Alk Phos 126 IU/L, total bilirubin 2.0 mg/dL, AST 63 IU/L, ALT 58 IU/L, tumor markers showed AFP 226 ng/mL (normal 0.0–8), CA 19-9 959 unit/mL (normal 0–35) and carcinoembryonic antigen (CEA) 3.9 ng/mL (normal 0–3). Hepatitis C antibody was reactive and Hepatitis B core AB negative. CAT-scan of the abdomen revealed a 1.3 cm mass in the head of the pancreas with intrahepatic and extrahepatic ductal dilatation (Fig. 1a). MRI of the abdomen showed a 3.7 cm mass in segment VI of the liver (Fig. 1b). ERCP with bile duct brushings was performed and consistent with malignancy. EUS demonstrated a 2.6 cm mass in the head of the pancreas with portal vein involvement. Ultrasound guided biopsy of the liver was consistent with HCC. (Fig. 2). Routine staging CT scan of the chest showed a prominent 2.1 cm pre-tracheal lymph node. Endobronchial ultrasound guided-fine needle aspiration (FNA) of this lymph node showed no evidence of malignant cells.

(a) CT scan of the abdomen showing pancreatic mass, solid arrow. (b) MRI of the abdomen showing segment six hepatic lesion, solid arrow.
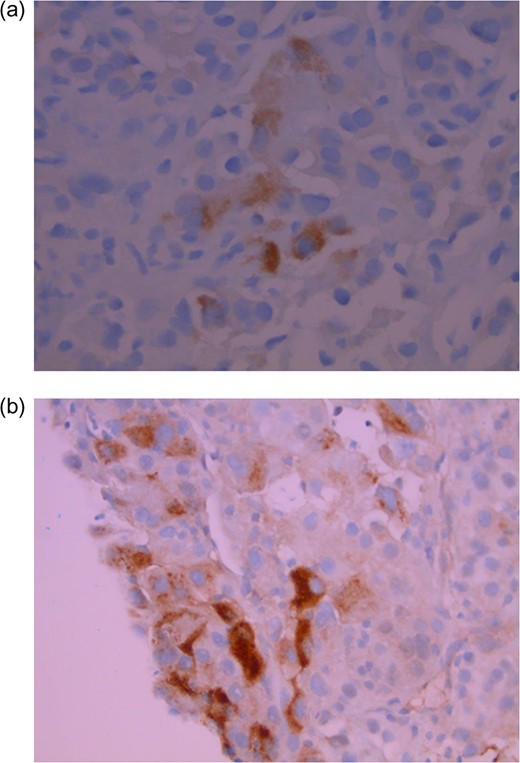
Tumor cells in cell block (FNA specimen) are positive for hepatocyte specific antigen (a) and alphafetoprotein (b) (magnification ×40).
Given the concern for portal vein involvement on EUS the pancreatic head lesion was deemed borderline resectable and a neoadjuvant approach was preferred. Prior to initiation of chemotherapy a staging laparoscopy and liver biopsy was performed. At operation there was no evidence of peritoneal carcinomatosis, metastatic disease or gross liver cirrhosis. On final pathology the liver lesion stained positive for alphafetoprotein (AFP) and hepatocyte specific antigen (HSA) supporting the diagnosis of a primary hepatocellular carcinoma. The uninvolved liver had no evidence of cirrhosis. The patient received neoadjuvant FOLFIRINOX followed by re-imaging. Repeat CT scan showed no evidence of disease progression. Pancreaticoduodenectomy with synchronous liver resection was offered. A classic Whipple procedure was performed with a duct to mucosal pancreatico-jejunostomy. A parenchyma-sparing segment VI non-anatomic liver resection was then performed. She was discharged home on post-operative Day 6. Pathology revealed a 6 cm poorly differentiated hepatocellular carcinoma (Fig. 3) and a 1 cm intra-ampullary carcinoma extending into proximal stomach and distal bile duct.
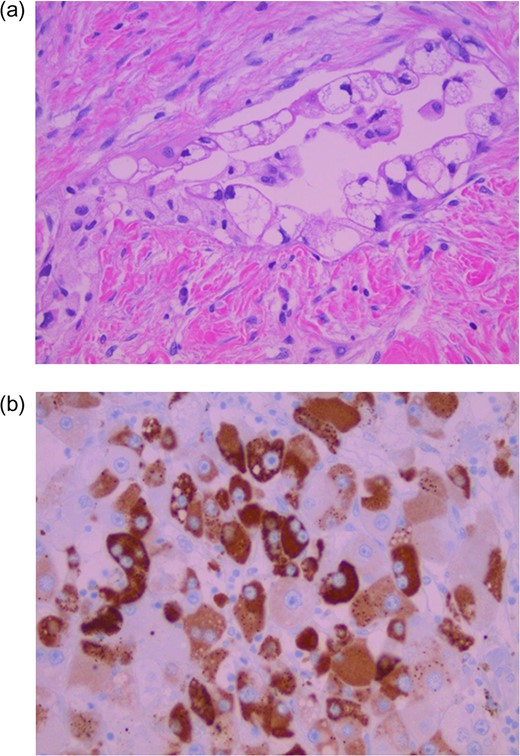
Adenocarcinoma with foamy cytoplasm invading dense stromal tissue (a). Tumor cells are positive for hepatocyte specific antigen (b) (magnification ×40).
DISCUSSION
Synchronous malignancies are defined as those that present simultaneously or within a 6-month period of each other. The diagnosis of synchronous malignancies of hepato-pancreatico-biliary origin is rare. Operable primary ampullary and liver cancer is even less common.
Differentiating ampullary carcinoma from other periampullary malignancies may be clinically as well as pathologically difficult. Ampullary cancers are uncommon and account for 15–25% of cancers in the periampullary region. Overall, 5-year survival after resection of ampullary cancer is superior to that of pancreatic cancer (43.3 vs 7–27%, respectively) [4, 5]. Pancreatic head adenocarcinoma is however much more common and more likely to present with metastatic disease.
Hepatic lesions in the setting of a peripancreatic adenocarcinoma is metastatic until proven otherwise. While hepatocelluar carcinoma is the most common primary cancer of the liver it is usually found in the setting of liver cirrhosis, chronic hepatitis B or C infection or non-alcoholic fatty liver disease. Even though our patient was infected with hepatitis C, her hepatocellular carcinoma developed in a non-cirrhotic liver. The incidence of non-cirrhotic hepatocellular carcinomas in western countries can be as high as 19% [6].
HCC developing in a non-cirrhotic patient with chronic hepatitis C infection has been reported but is very rare [7]. The hepatitis C virus may generate gene products with carcinogenic potential. Accelerated liver fibrosis without frank cirrhosis has also been implicated in non-cirrhotic HCC [8].
In appropriate patients, surgical options for managing hepatocellular carcinoma include resection or liver transplantation depending on size, number and location of the tumors. Resection of a solitary hepatocellular carcinoma in a non-cirrhotic patient is associated with the best long term treatment results with a 5-year survival of 44–58%, significantly higher than the survival in the presence of cirrhosis 23–48% [9]. Recent studies have reported decreased local recurrence and increased time to recurrence with anatomic resection compared to non-anatomic for HCC. However, impact on overall survival has not been demonstrated [10]. This patient presented with two relatively aggressive malignancies. An anatomic liver resection may not have impacted her overall survival but could have potentially added time and morbidity to the operation and therefore a non-anatomic liver resection was performed.
Care should be taken to rule out metastatic disease in patients with synchronous malignancies particularly when one of the lesions is hepatic. In this case the possibility of synchronous intra and extrahepatic biliary tumors was not considered given the radiographic characteristics of the hepatic lesion. The MRI revealed a hyperintense lesion, heterogeneous enhancement with central washout and delayed capsular enhancement, consistent with primary hepatocellular carcinoma.
Preoperative biopsy of the hepatic lesion stained positive for AFP and HSA supporting the diagnosis of a primary hepatocellular carcinoma.
Synchronous ampullary and hepatocellular carcinoma has not been reported in the literature previously. There have been reports of synchronous unresectable pancreatic and hepatocellular carcinomas [3]. We believe this is the first report of synchronous resectable ampullary and hepatocellular carcinomas.
The patient has recovered well from surgery. She has completed adjuvant chemotherapy as well as sofosbuvir and daclativir for hepatitis C. At 1 year after diagnosis she is without evidence of recurrent disease.
CONFLICT OF INTEREST STATEMENT
None declared.



