-
PDF
- Split View
-
Views
-
Cite
Cite
Akash Chitrakar, Kajan Raj Shrestha, Uttam Krishna Shrestha, Middle aortic syndrome with renal artery stenosis, Journal of Surgical Case Reports, Volume 2017, Issue 9, September 2017, rjx177, https://doi.org/10.1093/jscr/rjx177
Close - Share Icon Share
Abstract
A 39-year lady referred to Vascular Surgery OPD from Cardiology with uncontrolled hypertension, non- functional left kidney and absent bilateral femoral pulses. Investigations revealed middle aortic syndrome with non-functional left kidney with bilateral renal artery stenosis. She successfully underwent bypass of stenotic segment with polyester graft from descending thoracic aorta to left common iliac artery with reverse saphenous vein graft interposed between polyester and right renal artery.
INTRODUCTION
Middle aortic syndrome (MAS) is a clinical condition caused by segmental narrowing of the abdominal or descending thoracic aorta with high propensity for both visceral and renal artery involvement [1]. It is a rare disease accounting for 0.5–2% of all the cases of aortic stenosis [2]. It may be congenital due to defect in fusion of embryonic dorsal aorta during 4th week of gestation or acquired, associated with conditions like Takayasu disease, Neurofibromatosis, Fibromuscular dysplasia or Retro-peritoneal fibrosis [1, 3].
The most common clinical presentation of MAS is uncontrolled hypertension, followed by headache, claudication, dyspnea, abdominal angina and failure to thrive [4]. If left untreated, most patients with MAS die before the age of forty from complications like myocardial infarction, heart failure, intracranial hemorrhage and aortic rupture [1].
CASE REPORT
A 39-year lady presented in our OPD being referred from Cardiology for uncontrolled hypertension, absent bilateral femoral pulses and renal angiogram revealing bilateral renal artery stenosis (99%) and abdominal aorta stenosis (99%) (Figs 1–4).
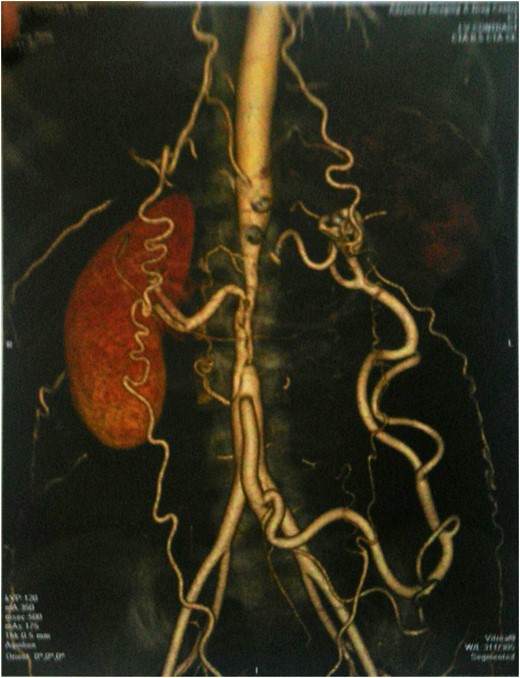
CT angiogram showing narrowing of abdominal aorta from origin of SMA up to IMA with multiple large collaterals, narrowed right renal artery and significantly narrowed left renal artery with poor enhancement of renal parenchyma.
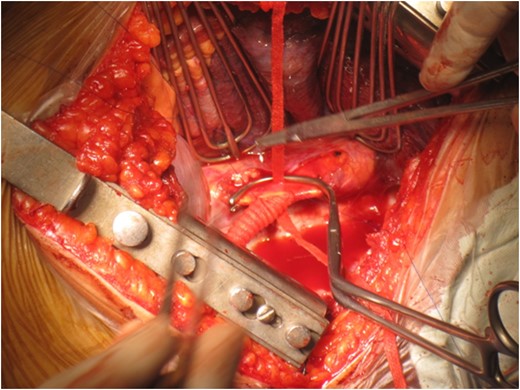
Anastomosis between descending thoracic aorta and polyester graft.
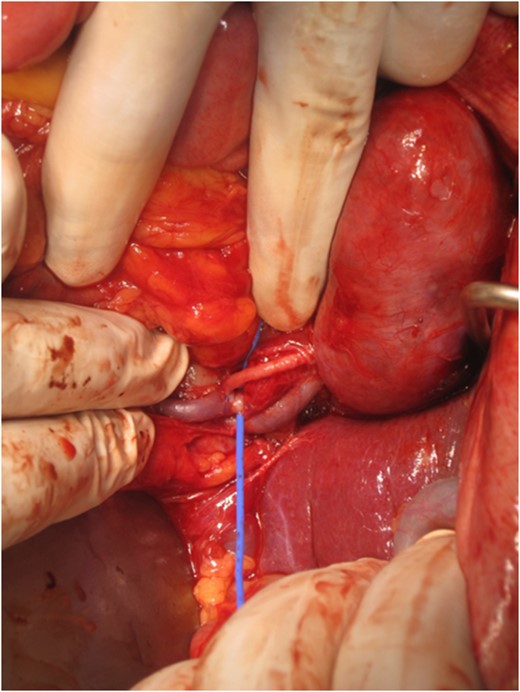
Following anastomosis between thoracic aorta and polyester graft an anastomosis was made between the graft and left common iliac artery (picture not provided). Reverse saphenous vein graft was harvested and anastomosed between the polyester and the right renal artery distal to the site of narrowing (shown in the provided picture).
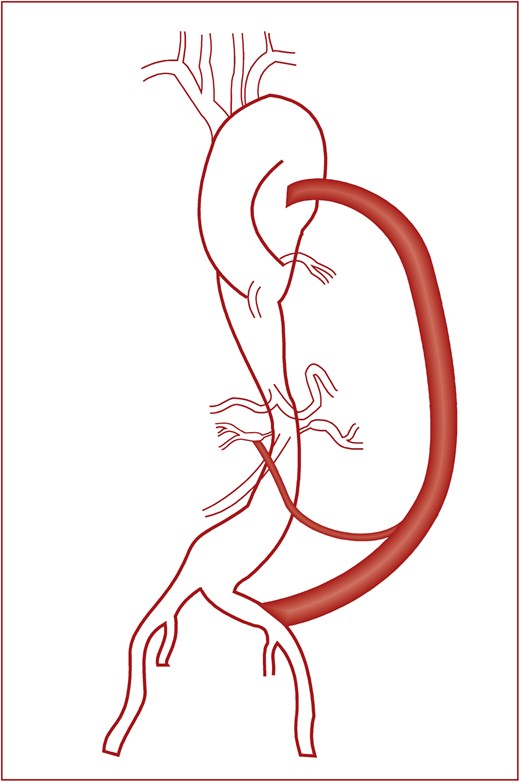
It is a pictorial representation of the entire operative procedure that we hope would give a clearer picture. It shows the graft between the descending thoracic aorta and left common iliac artery and reverse saphenous vein graft between the polyester graft and right renal artery.
She had a history of intermittent claudication for past 15 years and a known hypertensive for 9 years currently taking combination therapy of atenolol, amlodipine and thiazide diuretic.
On examination her radial pulse was 80 beats per minute,blood pressure was 160/80 mm hg both arms, bilateral femoral pulses were absent, and renal bruit was heard on right side.
Her routine hematological and biochemical parameters were normal. USG abdomen showed small left kidney and hypertrophied right kidney. Echocardiography was normal with EF = 65%. CT Angiogram revealed narrowing of the abdominal aorta from the level of origin of SMA up to IMA involving 6 cm long segment of the aorta, right renal artery was narrowed, left renal artery was significantly reduced in caliber with poor enhancement of renal parenchyma. DTPA Renogram showed non visualized left kidney with normal functioning right kidney.
Based on history, clinical examination and investigations diagnosis of MAS with Bilateral renal artery stenosis with non-functioning left kidney was made. She was planned for surgical treatment. Intra-operatively, her left kidney was shrunken, SMA was dilated, and abdominal aorta below SMA to iliac bifurcation was stenosed.
She underwent bypass of stenotic segment by an 8 mm polyester graft interposed between Descending thoracic aorta and left common iliac artery in a side-to-end manner. Polyester graft to Right renal artery bypass was made by Reverse Saphenous Vein Graft in a side-to-end manner. The entire procedure took 190 min to complete.
Post-operative period was uneventful. Bilateral femoral pulses were palpable. Her Blood pressure gradually normalized over the duration of her stay. Her investigations including kidney function tests were within normal range. The patient was discharged on seventh POD. The patient was followed up weekly for 1 month then monthly for 6 months.
On her 6 month follow-up, the patient was doing fine and her initial symptoms of claudication had improved significantly. Her blood pressure was normal without use of any anti-hypertensives. Doppler showed good flow in right kidney with patent graft.
DISCUSSION
Although the first description of MAS was given by Sen et al. in 1963 [5], most reports on MAS have been on congenital cases in children with only few cases being reported on adults with other etiologies. MAS commonly involves Abdominal aorta (97%), most common site within abdominal aorta being suprarenal (29%), followed by suprarenal to infrarenalstenosis (12%), renal artery is the most common extra-aortic vessel involved (66%) [4].
The treatment of MAS can be medical, endovascularor surgical. Medical management is to control hypertension and acute phase of aortoarteritis prior to definite surgical or endovascular therapy [1]. Indications of surgery include uncontrolled hypertension, lower limb claudication, involvement of kidneys and mesenteric ischemia [1]. Surgical repair depend upon the anatomy of lesion and involvement of visceral arteries. Surgical techniques include aorto-aortic bypass, patch aortoplasty, renal artery and visceral artery reconstruction [1].
Mid and long-term results indicate that in at least 70% of hypertensive patients who undergo reconstructive surgery, hypertension is either improved or cured after surgery [6, 7].
In one of the earliest series by Debakeyetal [8] on 16 patients with abdominal aortic coarctation and renal artery stenosis, severe hypertension was the most common presentation. All patients underwent aorto-aortic bypass with a polyester tube graft, except one in whom patch aortoplasty was performed. Renal artery stenosis was managed by reverse aorto-renal bypass with autogenous saphenous vein (children) or synthetic conduit, or both. Two patients underwent nephrectomy at the time of primary procedure. No deaths were reported. Five years after surgery, all patients remained normotensive and free of symptoms. Kim et al. [9] reported that 10 adult patients diagnosed with MAS caused by Takayasuarteritis who underwent surgical treatment. Indications for operation were uncontrolled hypertension in six patients and lower extremity claudication in four. Eight aortic bypasses, one supraceliac aortic interposition graft and one bilateral aorto-renal bypass were performed. Adjunctive renal bypass with saphenous vein graft and IMA reimplantation were performed simultaneously. Hypertension was cured or improved in five of the six patients, and lower extremity claudication improved in all of them. With a median follow-up of 60 months all the aortic bypasses were patent and one adjunctive renal artery bypass graft with aortic bypass was occluded 29 months post-operatively.
In our case, the patient was a 39 years old lady with involvement of long segment of abdominal aorta from suprarenal to infrarenal region and bilateral renal arteries. We performed aorto-iliac bypass for the long stenotic segment and bypassed the right renal artery. Claudication improved post-operatively and hypertension was cured.
CONFLICT OF INTEREST STATEMENT
None declared.



