-
PDF
- Split View
-
Views
-
Cite
Cite
Christopher J Down, Lalit Kumar, Sukhpal Singh, Darmarajah Veeramootoo, A unique complication of self-expandable metal stent placement in malignant duodenal obstruction, Journal of Surgical Case Reports, Volume 2017, Issue 9, September 2017, rjx169, https://doi.org/10.1093/jscr/rjx169
Close - Share Icon Share
Abstract
Intestinal obstruction is a common complication in patients with advanced gastrointestinal malignancies. In the last two decades, endoscopic placement of duodenal stents has become a mainstay of palliative treatment in patients with unresectable obstructive duodenal pathology. Self-expandable metal stents have been reported to have excellent success rates, besides dramatically improve the patient’s quality of life by reinstating the oral feeding ability. Re-intervention rates remain high, commonly as a consequence of tumour ingrowth resulting stent occlusion. We describe a unique case of duodenal stent obstruction secondary to impacted gallstones. To the best of our knowledge, this is the first case described in the literature and should alert clinicians to this unusual complication.
INTRODUCTION
Intestinal obstruction is a common complication in patients with advanced gastrointestinal malignancies. In the last two decades, endoscopic placement of duodenal stents has become a mainstay of palliative treatment in patients with unresectable obstructive duodenal pathology. Self-expandable metal stents (SEMS) have been reported to have excellent success rates, besides dramatically improve the patient’s quality of life by reinstating the oral feeding ability. Complications of such stents include obstruction, migration, perforation and stent fracture [1].
We describe a unique case of duodenal stent obstruction. To the best of our knowledge, this is the first case described in the literature and should alert clinicians to this unusual complication.
CASE REPORT
We report the case of a 78-year-old man, with locally advanced (pT4), moderately differentiated duodenal cancer diagnosed fourteen months previously. He underwent a palliative duodenal stent (NitiS) placement across D3 2 months following his diagnosis and commenced 10 cycles of chemotherapy (FOLFOX). At the time of his initial diagnosis, he was found to have large stones and sludge within the gallbladder. A subsequent biliary obstruction, noted 1 month following placement of the duodenal stent, necessitated the deployment of a metal biliary stent.
The patient presented with a 1-week history of vomiting and epigastric pain without any overt signs of sepsis. His blood tests did not reveal any abnormality apart from deranged liver function tests, showing mild elevation of serum bilirubin (38 μmol/l), with an obstructive picture (ALP 373IU/L).
A CT scan (Fig. 1) reported duodenal obstruction secondary to tumour ingrowth. However, a subsequent gastrografin swallow performed 2 days later showed free passage of contrast through the duodenal stent without any hold up. On the basis of imaging result the patient was allowed to resume oral intake. During the admission the bilirubin started to increase and therefore on Day 18 of his admission (Bilirubin 130 μmol/l), a magnetic resonance cholangiopancreatography was performed. This revealed bilobar intrahepatic biliary duct dilatation without an obvious aerobilia, in keeping with biliary obstruction. The patient underwent an endoscopic retrograde cholangiopancreatography (ERCP) that demonstrated tumour ingrowth at the lower end of the biliary stent. An uncovered stent was successfully deployed to relieve the biliary obstruction.

CT scan showing gastric and duodenal dilatation down to the level of the stent suggesting obstruction at this level.
On Day 7 post-ERCP, the patient developed severe vomiting and was unable to tolerate oral intake. A repeat gastrografin swallow at this stage revealed duodenal obstruction. The patient was kept nil-by-mouth and the stomach was decompressed with a nasogastric tube. Gastroscopy (Fig. 2) was performed the following day and revealed two large calculi as the cause of stent blockage. One of the stones was impacted at the level of D2 obstructing the duodenal stent, with the second stone lying free above it.
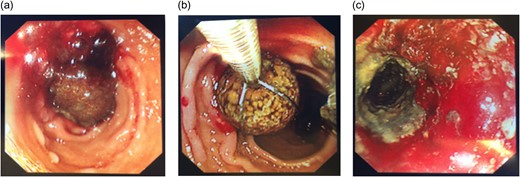
Gastroscopy showing the impacted stone (a), stone retrieval (b) and a patent lumen post procedure (c).
Retrieving these stones proved a challenge in many aspects; their size (Fig. 3; 3 cm diameter) and hard consistency made them difficult to manipulate. Furthermore, fragmenting them with lithotripsy would have created multiple fragments risking further obstruction. We therefore elected to retrieve each stone individually using an endoscopic snare.
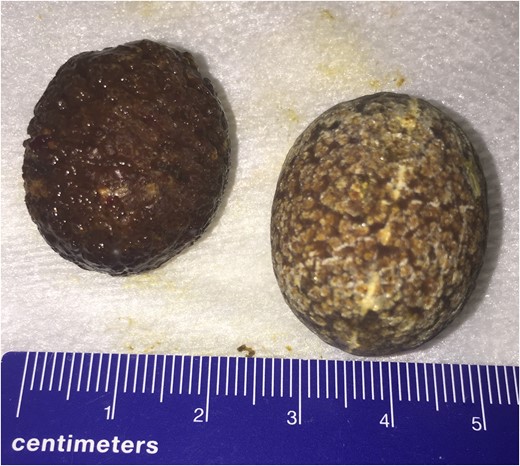
Following the successful retrieval of the stones, the duodenal stent was noted to be patent without any evidence of tumour ingrowth. Biochemical analysis confirmed these were cholesterol stones, compatible with gallstones. Over the course of next 3 days, the patient recovered completely and was discharged home having restarted a normal diet. The patient has responded well to treatment and 4 months following discharge, he remains asymptomatic.
DISCUSSION
Patients with malignancy of the upper gastrointestinal tract commonly develop duodenal or biliary obstruction complicating their clinical course. Our standard practice is stenting of primary duodenal obstruction as a joint procedure with an intervention radiologist under propofol sedation. ERCP and stenting is first attempted for solitary biliary obstruction and if unsuccessful, we proceed to percutaneous transhepatic cholangiography (PTC). In dual obstruction, we stent the biliary system first and for secondary biliary obstruction after duodenal stenting, we favour PTC.
The deployment of SEMS has thus become the treatment of choice for patient with non-operable malignant gastric outflow obstruction. Whilst SEMS are well tolerated and offer good clinical success rates; our re-intervention rate is similar to literature reports (30%), and remain high [2]. The commonest reason is stent occlusion secondary to tumour ingrowth [3]. However, more often than not patients are consumed by their advanced disease; but benefit from a better quality of life after stenting. On rare occasions, after careful planning and with expert radiologist, repeat stenting through stents is attempted, with surgical bypass as a bail out option.
This case demonstrates a rare cause of stent occlusion secondary to impacted gallstones. The mechanism underlying this pathogenesis is difficult to establish. We know that a cholesterol stone was impacting the duodenal stent causing obstruction. Whether there is a causal relationship between the deployments of biliary stent 7 days prior to the patient developing duodenal obstruction remains questionable. Given there was no evidence of bile duct stones on MRCP prior to ERCP, it is unlikely that such sizeable stones would be able to pass through the newly deployed biliary stent.
An alternative opinion was that the patient developed a cholecysto-duodenal fistula allowing for the migration of stones. Similar pathogenesis is seen in Bouveret’s syndrome, where GOO is caused by impacted gallstones within the duodenum. This case parallels the challenge in subsequent diagnosis and management. Such pathogenesis, in the context of a recently deployed duodenal stent, has not previously been reported. Factors favouring this theory include the size of the gallstones (2–3 cm), the chronic history of biliary disease secondary to his duodenal cancer, and old age. Nonetheless, neither MRCP nor ultrasound could identify any evidence of a cholecysto-duodenal fistula and therefore this remains unproven.
To the best of our knowledge, this is the first reported case of duodenal stent occlusion secondary to an impacted gallstone. Whilst not a common occurrence, this case does provide an insight into the challenges faced by clinicians dealing with these complex patients. Though exceptional, flexibility of endoscopic approach with multi-disciplinary back up and technical expertise offers the potential for novel solutions.
ACKNOWLEDGEMENT
None.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
FUNDING
We have no sources of funding to declare at this time.
CONSENT FOR PUBLICATION
The consent was obtained from the patient.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.



