-
PDF
- Split View
-
Views
-
Cite
Cite
Cameron G. Hanson, Todd B. Proctor, Ethmoid malformation associated with pediatric nasal polyposis and allergic fungal sinusitis, Journal of Surgical Case Reports, Volume 2017, Issue 6, June 2017, rjx099, https://doi.org/10.1093/jscr/rjx099
Close - Share Icon Share
Abstract
A 17-year-old female with allergic fungal sinusitis and nasal polyposis presented with epistaxis in the emergency room. On examination, right-sided proptosis and irregular nasal obstruction were observed in the right nasal cavity. CT imaging revealed massive right-sided polyposis and significant ipsilateral malformation with boney architecture preservation of the ethmoidal labyrinth and lamina papyracea. The patient was treated surgically with symptomatic improvement. These findings indicate a unique malformation of the ethmoid while the patient was in development. To the authors’ knowledge, this anatomical malformation has not been previously described in the literature. Physicians should implement diagnostic procedures early if nasal polyposis and allergic fungal sinusitis is suspected in pediatric patients, especially with periocular involvement, to mitigate the risk of boney malformations of the sinuses.
INTRODUCTION
Nasal polyposis and allergic fungal sinusitis (AFS) can be a severe condition, especially in the pediatric population. Early detection and surgical management is key to reducing potential comorbidities. We describe a novel case of malformation of the ethmoid sinus and lamina papyracea due to unilateral nasal polyposis and AFS.
CASE REPORT
A 17-year-old female with history of progressive nasal obstruction, purulent drainage, cough and anosmia over 8 months, was diagnosed with a nasal polyp by her primary doctor and was treated with azithromycin, and montelukast sodium with negligible relief. Intranasal steroids were also not effective. Her past medical history included insulin resistant diabetes, allergic rhinitis, unilateral proptosis of the right eye and Hashimoto’s thyroiditis. Allergy testing had been done 12 years prior.
She presented to the emergency room with epistaxis, prompting an otolaryngology referral.
On examination, the patient’s nasal septum was deviated to the left, irregular polyps were completely occluding the right nasal cavity, and there was unilateral right-sided proptosis. Sweat chloride [1] test was negative. A computed tomography (CT) scan of the sinuses was ordered.
The results of the CT indicated complete opacification of the frontal, ethmoidal, sphenoidal and maxillary sinus on the right side with hyper-dense intraluminal soft tissue filling the sinus cavities. Significant widening of the ostiomeatal complex was observed (Fig. 1). Soft tissue from the right maxillary sinus extended into the right side of the nasal cavity. Extensive changes in the right ethmoidal labyrinth were also discovered. The intact lamella of the middle turbinate and lamella of the bulla ethmoidalis extended further laterally when compared to the left side, and lamina papyracea was protruding into the orbit (Figs 1 and 2). Options were discussed and endoscopic CT guided surgery was recommended.
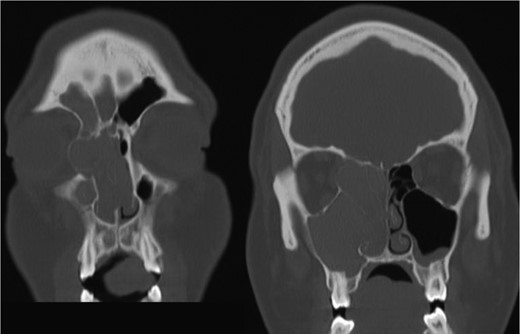
Coronal CT image indicating extent of soft tissue in the right nasal passage, malformation of the right lamina papyracea, and complete opacification of the right maxillary, ethmoidal and frontal sinus.
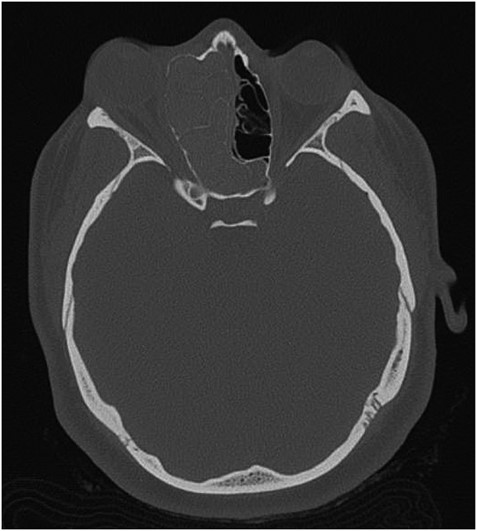
Axial CT image indicating widening of the ostiomeatal complex with malformation of the right ethmoid.

Axial CT view of the ethmoid labyrinth with the left side super imposed on the right side over the midline for comparison.
Findings at surgery included extensive polyps and concretions filling all of the right side sinuses. The right lamina papyracea was ~2 cm lateral. Biopsies from both the right and left sinuses demonstrated focal fungal elements including spores and hyphae.
The patient had an uneventful postoperative course. The family decided against standard use of oral corticosteroids [2–4] due to her Juvenile diabetes. Allergy management was recommended. Five weeks post-operatively, she had significant improvement in breathing and perceived improvement in proptosis, along with alleviated anosmia. At 10 weeks post-operatively, the patient perceived her proptosis to be nearly completely resolved and there was no sign of infection reoccurrence. The patient was informed she may need oculoplastic surgery to fully correct the malformed bone structure.
DISCUSSION
AFS is a known risk factor for development of nasal polyps [5, 6]. Incidences of AFS causing unilateral proptosis have also been described in the literature [7, 8]. The findings from the current CT, however, indicate a unique developmental process. When compared to the patient’s left side, the extent is easily seen (Fig. 3). In consideration of the preservation of the ethmoid architecture along with the patient’s age, it appears that due to the severity and duration of the polyposis and AFS, the ethmoidal labyrinth malformed while still in development. Contrastingly, in cases of several nasal polyposis, including those with ocular involvement, bone erosion and destruction are most frequently seen with respect to changes in bone anatomy [9]. Chronic remodeling of the ethmoid bone has been described in venous malformations [10], however, cases of nasal polyps leading to bone malformation are significantly underrepresented in the literature. CT imaging proved the most valuable diagnostic tool in examining the extent of the proptosis secondary to polyposis, as well as describing the changes in the ethmoid labyrinth structure. Surgical approach proved effective in reducing the patient’s symptoms, as well as confirming the etiology of the unilateral proptosis.
In pediatric patients, nasal polyposis and AFS can precipitate secondary concerns. The current case indicates that these combined diagnoses may lead to malformations of the ethmoidal labyrinth. As such, CT diagnostic measures should be implemented early if nasal polyposis or AFS is suspected in juvenile cases, particularly with periocular involvement.
ACKNOWLEDGMENTS
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Signed consent was obtained from the patient.
CONFLICT OF INTEREST STATEMENT
None declared.



