-
PDF
- Split View
-
Views
-
Cite
Cite
Akshay Yadhati, Swamy Kurra, Richard A. Tallarico, William F. Lavelle, Lumbar vertebral body and pars fractures following laminectomy, Journal of Surgical Case Reports, Volume 2017, Issue 2, February 2017, rjx007, https://doi.org/10.1093/jscr/rjx007
Close - Share Icon Share
Abstract
A 56-year-old alcoholic male incurred L5 vertebral body and bilateral L4 pars fractures with progressive L4 on L5 anterolisthesis following low-energy falls while intoxicated. Recently, he had a L3–S1 laminectomy for lumbar spinal stenosis with claudication. Preoperative imaging and radiographs were negative for pars defects and instability, so an isolated decompressive surgery was performed. Following low-energy falls, his outpatient work-up revealed fractures through the bilateral L4 pedicles and posterior third of L5 vertebral body, with recurrence of axial back pain and bilateral lower extremity radiculopathy. He underwent revision decompression from L4–S1 and posterior instrumented fusion with transforaminal lumbar interbody fusion performed at each revised level. His axial back pain and radiculopathy improved postoperatively. Instability of a lumbar spine fracture pattern can be due to the remote or prior iatrogenic disruption of the posterior ligamentous complex. Our patient benefitted from surgery and his low back pain was resolved.
INTRODUCTION
The Denis’ three-column theory [1] presented in 1983 as it relates to thoracolumbar spinal injuries is a well-supported and trusted concept. It raised the importance of the posterior ligamentous complex (PLC). Over the years, this principle has been upheld by multiple studies; most pointedly by the development of the thoracolumbar injury classification and severity score [2]. The system and marked importance of the PLC guide the evaluation and treatment of spine injuries. As providers, we typically account for the combination of injuries and the patient presentation after a single traumatic event without prior disruption to the osseous or soft-tissue structures. We are faced with a complex clinical scenario when the posterior elements have been removed following a multilevel decompression for symptomatic lumbar spinal stenosis and that patient then incurs an injury to the remaining posterior osseous structures and vertebral body over a year after index surgery.
This case report describes the case of a patient who underwent a revision decompression from L4–S1 and posterior instrumented fusion with a transforaminal lumbar interbody fusion (TLIF) performed at each of these revised levels after a series of low-energy falls. The patient provided written informed consent for print and electronic publication of this case report.
CASE REPORT

Standing lateral lumbar radiograph obtained 2 weeks following the patient's initial lumbar surgery (L3–S1 laminectomy). No instability is noted on the postoperative image.

Standing neutral lateral lumbar radiograph obtained 17 months following the patient's L3–S1 laminectomy. The patient is now dealing with a Grade 1 anterolisthesis of L4 on L5, with a mild degree of retrolisthesis at each of the cranial levels depicted.
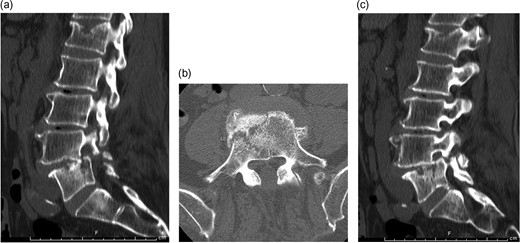
Median, parasagittal and axial images from a lumbar CT scan obtained following review of the patient's lumbar radiographs. (a) Sagittal CT demonstrating vertebral body split. (b) Axial CT demonstrating vertebral body fracture at L5. (c) Sagittal CT demonstrating pars fractures at L4.

Standing neutral lateral lumbar radiograph obtained the day following the patient's L4–S1 revision decompression and posterior instrumented fusion with TLIF performed at each of these revised levels. A moderate correction of the prior L4-5 anterolisthesis was achieved and the patent's spine and construct appear stable.
DISCUSSION
Subsequent instability due to excessive excision of the posterior elements during lumbar decompression is a known complication. Moreover, fracture of the remaining posterior elements is an important aspect of the differential diagnosis in evaluating patients with persistent or recurrent symptoms following decompression. Reports document the incidence of fracture to the inferior articular process as well as the pedicle following decompression. The advent and evolution of computed tomography (CT) has improved our understanding of this complication [3–5]. Lumbar pedicle stress fractures, either prior to or following surgery, have also been documented as a source of pain and instability.
Doita et al. documented a case of a 57-year-old male patient with bilateral L4 pedicle stress fractures in the setting of multilevel lumbar spinal stenosis and severe L4-5 degeneration. An all-posterior L3–S1 decompression and fusion was performed and the patient experienced significant relief of symptoms [6]. Maurer et al. presented a case where a disruption to the posterior elements as minimal as a laminectomy required for a micro-discectomy can potentially result in subsequent stress injuries of the pedicles and instability at the operative level [7].
Pedicle stress fractures have also been documented following revision surgery in which removal of pedicle screw instrumentation was performed in the setting of a mature fusion mass. Ha et al. [8] detailed a case of a 62-year-old man that underwent a L1–3 laminectomy and fusion and removal of prior L3–5 instrumentation for adjacent segment disease; and 6 years after a L3–L5 decompression and fusion for lumbosacral instability. Roughly 1 year following this revision surgery, the patient began experiencing significant low back pain, exacerbated by extension of the lumbar spine. Radiographs were unremarkable, but bilateral L4 pedicle fractures were diagnosed on CT and bone scans. The patient declined reinstrumentation. Macdessi et al. [9] presented a similar case of a patient who incurred bilateral L4 pedicle stress fractures after removal of prior instrumentation in the presence of a mature fusion mass from L4–S1.
There is a trend toward minimally invasive lumbar decompression for the treatment of lumbar stenosis. Ivanov et al., in this biomechanical study, observed increases in stresses at both the pars interarticularis and the inferior facet after limited decompressions and suggested surgeons should be aware of possible stress fractures [10]. Minimally invasive lumbar decompression procedures are still developing. There is little research about clinical stress fractures after these procedures that have been reported in the English literature.
The incidence of fracture to the vertebral body in isolation, or in addition to an injury to the remaining posterior elements, is not well documented in the literature. It is reasonable to view this injury as part of a spectrum beginning with a stress injury to the remaining posterior elements which then progresses to complete fracture of the pedicle with subsequent listhesis and possible contact of adjacent vertebral bodies. In our patient, the initial injury was possibly compounded by multiple low-energy falls. As a result of the patient's combined injury morphology and subsequent progression of listhesis, it was felt that revision decompression with an interbody fusion was reasonable. He has benefitted from surgery and his symptoms resolved.
REFERENCES
- diagnostic radiologic examination
- back pain
- lameness
- fractures
- laminectomy
- low back pain
- poly(adp-ribose) polymerases
- outpatients
- preoperative care
- radiculopathy
- spinal fusion
- surgical procedures, operative
- diagnostic imaging
- leg
- surgery specialty
- intoxication
- lumbar spinal stenosis
- lumbar spine fractures
- vertebral body
- third lumbar vertebra



