-
PDF
- Split View
-
Views
-
Cite
Cite
Kazuhiko Ishimaru, Kanta Araki, Tsuneyuki Nakamura, Yoshiki Sawa, An alternative technique for direct implantation of an anomalous left coronary artery arising from the pulmonary artery with complex coronary arteries, Journal of Surgical Case Reports, Volume 2016, Issue 9, September 2016, rjw161, https://doi.org/10.1093/jscr/rjw161
Close - Share Icon Share
Abstract
A 2-month-old patient with anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA) underwent an alternative repair involving coronary transfer with the bay window technique because of the very short left main coronary trunk. This procedure is a clinically relevant and feasible technique for ALCAPA with such a delicate coronary artery anomaly.
Introduction
The direct aortic implantation of an anomalous coronary artery into the ascending aorta is widely acceptable as the method of repair for anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA) [1], but it may not be possible for unusual coronary artery anatomy. In the present case, a dual-coronary system was created for ALCAPA with a very short left main coronary trunk using the bay window technique to prevent kinking and overstretching of the translocated coronary artery.
Case report
A 1-month-old female was admitted to our institution with high fever, cough and poor feeding caused by respiratory syncytial virus infection. Two-dimensional and color-flow Doppler echocardiography demonstrated a grossly hypokinetic and dilated left ventricle with mild-to-moderate mitral regurgitation, in addition to reversal of flow from the anomalous left coronary artery into the pulmonary artery (PA) that constituted a left-to-right shunt. Cardiac catheterization and computed tomography coronary angiography showed the single right coronary arising from the aorta and retrograde filling of the left coronary artery with a very short main coronary trunk that originated from the rightward posterior sinus of the PA (Fig. 1).
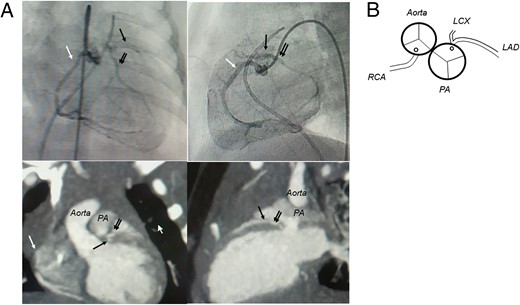
(A) Preoperative cardiac catheter angiography, contrast CT and (B) the schema of the coronary pattern. The aorta is located right and posterior to the PA, and the left coronary artery with a very short main coronary trunk originates from the rightward posterior sinus of the PA (LAD: left anterior descending artery, black arrow; LCX: left circumflex artery, double arrows; RCA: right coronary artery, white arrow).
Cardiopulmonary bypass with bicaval and distal aortic cannulation and mild hypothermia were established. Both pulmonary arteries were dissected and looped. Cardioplegic spikes were inserted into both the ascending aorta and the pulmonary trunk (PT), and a left side vent was placed through the right upper pulmonary vein. The aortic crossclamp was placed high, and cardioplegic solution was delivered simultaneously into the aortic root and the PT using a bifurcated cardioplegia delivery system to maximize protection of the left ventricle, after bilateral pulmonary arteries were snared tightly to prevent perfusion steal into the pulmonary bed from the PA cannula. The ascending aorta was transected at a high level more than 10 mm above the sinotubular junction, and the main PA was transected just below the bifurcation. The left coronary artery originated from the rightward posterior sinus of the pulmonary sinus with a single orifice and a very short main trunk. The coronary button was harvested with a generous cuff of the pulmonary sinus wall, and the proximal portion of the coronary artery was mobilized with preservation of branches. A trap-door incision was made in the ascending aorta higher than the aortic commissure (Fig. 2A), and the coronary cuff was sewn with a 7-0 polypropylene suture, starting at the bottom of the J-shaped incision and the inferior end of the cuff. After partial resection of the superior edge of the J-shaped aortic flap, the superior excess cuff was folded inside and covered with the bay window-like bulged coronary channel (Fig. 2B). The proximal aortic stump was anastomosed to the ascending aorta with a 6-0 polypropylene suture. The anterior wall of the transverse section of the ascending aorta was anastomosed to the inner edge of the folded-down cuff (Fig. 2C). The defect in the main PA was reconstructed with a generous fresh autologous pericardial patch.
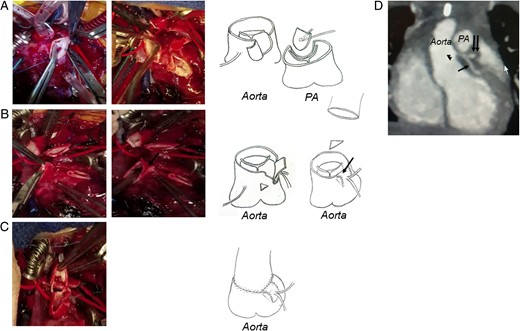
Intraoperative pictures and the schema of the operative procedure. (A) After the transection of both the aorta and PA, a large coronary button is excised and mobilized from the PA trunk. The trap-door incision is subsequently made in the aorta above the sinotubular junction. (B) The coronary cuff is sewn, and the superior excess cuff is folded inside and covered with the bulged coronary channel (black arrow) after partial resection of the superior edge of the J-shaped aortic flap. (C) The proximal aortic stump is anastomosed to the ascending aorta, and the anterior wall of the transverse section of the ascending aorta is anastomosed to the inner edge of the folded-down cuff. (D) Postoperative computed tomography coronary angiography shows the new coronary channel of the left coronary artery (arrow head) arising from the ascending aorta above the sinotubular junction (left anterior descending artery, black arrow; left circumflex artery, double arrows).
The patient's postoperative course was uneventful, and echocardiography revealed trivial mitral regurgitation after weaning off cardiopulmonary bypass. She had an uneventful postoperative recovery and no kinking and overstretching of the translocated left coronary artery (Fig. 2D).
Discussion
ALCAPA is a rare congenital anomaly that is usually lethal without surgical intervention. More recently, the concept of establishing a dual-coronary system has been advocated and widely accepted [2].
Kinking or overstretching of the translocated coronary artery is a crucial factor, and surgical techniques for ALCAPA repair are required to facilitate tension-free coronary transfer. Turley et al. [3] reported that direct aortic implantation was possible in all cases of ALCAPA, but we considered that one of the coronary patterns that is technically difficult to translocate includes a coronary artery with a short main system that could not be simply implanted without kinking or stretching. Ando et al. [4] reported that the use of trap-door technique on the aortic wall might involve minimal rotation of the coronary artery and be applicable for the majority of ALCAPA cases without kinking and overstretching of the coronary artery, obtaining ample space between the reconstructed PA and the LCA. In addition, Yamagishi et al. [5] reported that the bay window technique for transfer of complex coronary arteries with transposition of the great arteries could form a wider coronary pathway and subsequently maintain the spatial geometry and divergence angle of the coronary artery. The superior part of the coronary channel was covered with a folded-down coronary cuff, and it could be simultaneously led to form a large coronary channel and decrease the difference in caliber between the distal and proximal stumps of the aorta when reconstructing the ascending aorta.
In the present case with a very short left main trunk, the bay window technique was used for transfer of the coronary cuff, preventing kinking or stretching of the translocated coronary artery, because the spatial relationships and geometry of the translocated coronary cuff did not change after anastomosis between the distal and proximal stumps of the aorta. The processing of both the upper and lower ends of the anastomosis between the open door-like aortic wall and the coronary cuff used by the bay window technique provided a beneficial effect that maintained the spatial geometry and divergence angle of the coronary artery, because the upper part of the flap-like aortic wall door and the coronary cuff were sewn to match the inside wall, the upper part of the coronary flow pathway was consequently narrowed.
In conclusion, the bay window technique may be a useful adjunct method for the establishment of a dual-coronary system in ALCAPA with especially complex coronary anomalies.
Funding
Japan Society for the Promotion of Science.
Conflicts of interest statement
None declared.



