-
PDF
- Split View
-
Views
-
Cite
Cite
Kasra Razi, Duncan Light, Liam Horgan, Emergency repair of Morgagni hernia with partial gastric volvulus: our approach, Journal of Surgical Case Reports, Volume 2016, Issue 8, August 2016, rjw151, https://doi.org/10.1093/jscr/rjw151
Close - Share Icon Share
Abstract
Morgagni hernias are a rare form of congenital diaphragmatic hernias, thus there is paucity in literature about the diagnosis and management of the condition. We report an 83-year-old woman who presented with vomiting and a metabolic acidosis with a previous computed tomography diagnosis of Bochdalek's hernia. Diagnostic laparoscopy revealed a Morgagni hernia containing transverse colon, greater curvature of the stomach and a partial gastric volvulus. The hernia was reduced with the sac untouched, and the defect was closed with a composite mesh using tac fixation. The operation was done successfully in 45 minutes with no complications.
Introduction
Morgagni hernias are rare form of congenital diaphragmatic hernias (CDH) and represent 2% of all CDH with the majority being Bochdalek. In the acute setting, patients present with signs of obstruction or strangulation. In the chronic setting, patients are either asymptomatic or present with non-specific respiratory or upper gastrointestinal symptoms. However, the majority of cases are found incidentally during investigations of other conditions.
Case Report
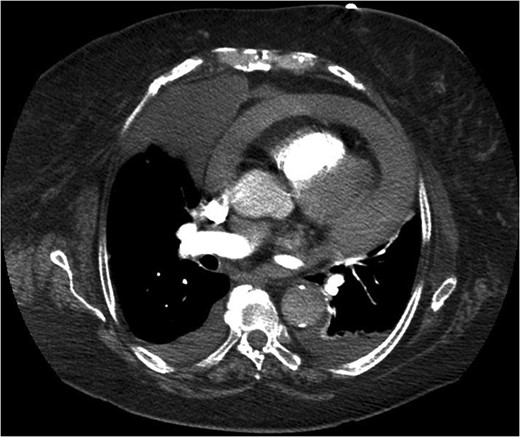
An 83-year-old woman presented to accident and emergency with sudden symptoms of abdominal pain and vomiting. She had presented a month earlier with similar symptoms and dysphagia, which had been ongoing for 2 weeks. Clinical examination had shown reduced air entry in the right lung and a normal abdomen. Chest X-ray showed consolidation in the lower right zone but with no symptoms or signs of a lower respiratory tract infection. She was taken under the care of the medical team and went on to have a computed tomography (CT) scan (Fig. 1) of her chest, which revealed a Bochdalek's hernia. Her symptoms settled, and she was discharged without a surgical review.
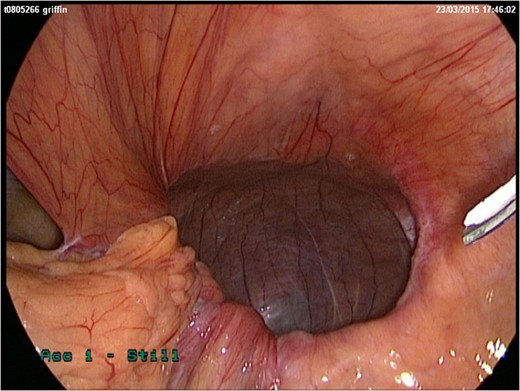
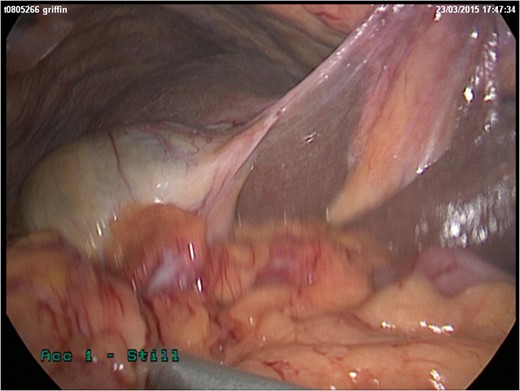
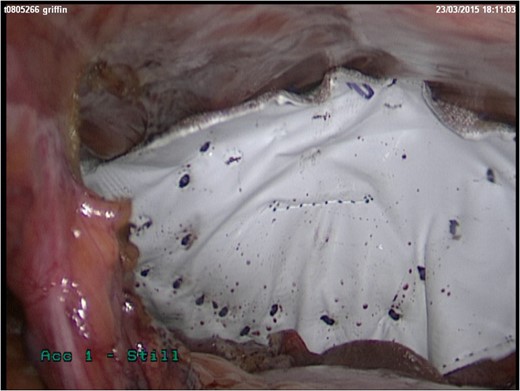
She represented later to our unit with recurrent vomiting. Her investigations revealed a raised lactate and acidosis on arterial blood gas. There was a concern for gastric ischaemia; the decision was taken to proceed to theatre. Given that she was haemodynamically stable with no peritonitis, we chose to operate using a laparoscopic approach. Surgery was performed through four laparoscopy (2 × 11 mm, 2 × 5 mm). A diagnosis of Morgagni hernia was made (Fig. 2). Inside the hernial sac was the transverse colon, the greater curvature of the stomach with a partial gastric volvulus (Fig. 3). The hernia was reduced with the viscera still viable but the sac could not be excised. The defect was repaired with a 6 × 10 cm composite mesh with an absorbable tic fixation on the diaphragm (Fig. 4). No drain was inserted, and the operation time in total was 45 minutes.
Discussion
Diaphragmatic hernias of Morgagni were first described in 1769 as anatomical defects in the anterior diaphragm that allow herniation of abdominal viscera into the thorax. They usually present in childhood with respiratory symptoms [1]. Incidental findings of this condition in adults are less common with only 81 asymptomatic cases reported in a recent review [2]. Symptomatic adult cases of Morgagni hernias are even rare with only 12 cases described [2]. Very few present with chest symptoms, the majority describing abdominal pain due to strangulation of the viscera. Of the symptomatic adult cases, the herniated viscera involve omentum, small bowel or stomach [2].
Presentation with non-specific respiratory or gastrointestinal symptoms makes clinical diagnosis difficult. Occasionally, these patients are initially admitted under the care of the medical team and referred late to the surgical team in more unstable conditions making management more difficult. It is important that patients presenting with a mixed signs and symptoms are assessed thoroughly including a review by both the medical and surgical team. CT is recommended as the gold standard investigation [3, 4].
In the acute setting, papers have suggested that laparotomy should be the method of choice but more recently there has been a shift to favour a laparoscopic approach [5, 6]. As in paraoesophageal hernias, the patient should be assessed for haemodynamic stability or signs of peritonitis [1, 7].
Various laparoscopic techniques have been reported; however, the optimal approach for the best outcome is still unknown due to the rarity of the condition. Given the favourable outcomes for laparoscopic giant paraoesophageal hiatal hernia repair, we would recommend that laparoscopy should be considered [7]. Previous case reports suggest repairing the defect using a mesh, while some favour suture repair [8, 9]. The choice of repair depends on the size of the defect, as larger defects would not generally be possible to repair with suture.
Conclusion
Early review of the patient by the surgical team is key in the patients’ outcome. In the acute setting, a CT scan should be the investigation of choice. Laparoscopic repair should be attempted where feasible. There is still debate between mesh versus suture repair, but the size of the defect and the surgeon's experience should determine the approach chosen.
Conflict of interest statement
None declared.
References



