-
PDF
- Split View
-
Views
-
Cite
Cite
Hasan Raza Mohammad, Waqar Bhatti, Anand Pillai, An unusual presentation of arteriovenous malformation as an erosive midfoot lesion, Journal of Surgical Case Reports, Volume 2016, Issue 8, August 2016, rjw146, https://doi.org/10.1093/jscr/rjw146
Close - Share Icon Share
Abstract
Erosive bony lesions are radiographic findings where localized bone resorption and cortical line breakage occurs. One less common cause of bone erosions is arteriovenous malformations (AVMs). This should always be included in the differentials for foot pain.
A 33-year-old gentleman presented with a 5-year history of chronic left foot pain. Clinical examination was unremarkable. Magnetic resonance imaging (MRI) and computerized tomography demonstrated erosive bone changes in the navicular, the intermediate and lateral cuneiforms bones and their corresponding metatarsal bases. An ultrasound and magnetic resonance angiogram demonstrated high signal showing the abnormal communication between metatarsal artery and vein at the site of most pain confirming the AVM. This was subsequently successfully treated with sclerotherapy.
Clinicians should be aware of the history, symptoms and signs of AVMs and consider the use of MRI with or without digital subtraction angiography in making a definitive diagnosis.
Introduction
Erosive bony lesions are a radiographic finding of localized resorption of bone often accompanied by cortical line breakage. Only a few conditions cause bone erosions, most commonly rheumatoid arthritis. Other causes include septic arthritis, psoriatic arthritis, tumours, metastases and granulomatous diseases. A less common cause of bone erosions is arteriovenous malformations (AVMs) [1].
A PubMed search using the search terms AVM, foot and erosion yielded no results. Although uncommon this important differential should be considered in foot pain presentations, and since many orthopaedic surgeons have not had routine exposure to AVMs, this diagnosis can easily be overlooked [2].
We present a case of a young gentleman presenting with left foot pain with imaging revealing an erosive midfoot lesion and the diagnostic difficulties encountered.
Case report
A 33-year-old Afro-Caribbean gentleman presented with a 5-year history of progressive chronic left foot pain. He had a road traffic accident in 2004, which resulted in plate fixation of his right femur but no history of direct impact or injuries to his left foot. He was otherwise fit and well.
He complained of metatarsal discomfort when weight bearing, eased by simple analgesics but would recur on stopping medication. The pain was sharp and stabbing in nature and worsened with activity, limiting his daily routine (Fig. 1).
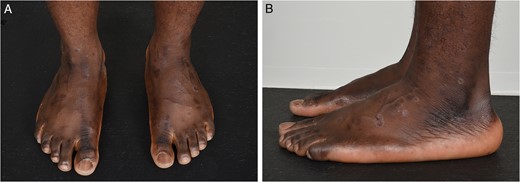
Anterior–posterior (A) and lateral views (B) of both feet. No obvious abnormalities were detected on general inspection.
On clinical examination, a full complement of pulses were present bilaterally with a normal capillary refill. On palpation, no sensory changes or midfoot pain was detected. All foot joints and the patients gait were unremarkable. Doppler ultrasound (US) showed good biphasic signals in pedal pulses with an ABPI of 1.12.
Left foot magnetic resonance imaging (MRI) scans demonstrated bony erosive changes (from 5 to 7 mm) in second and third tarsometatarsal joints and the navicular bone. The pattern of distribution made osteoarthritis from a prior accident, inflammatory arthritis and gout unlikely. Normal blood sugar levels ruled out diabetes and normal C-reactive protein and white cell count ruled out infective causes. The lack of signal dropout on fat saturation sequences raised suspicion of a synovial sheath tumour and biopsy was recommended. This was not conducted since going through normal bone could cause iatrogenic fractures, which in turn could destabilize the foot. Furthermore, if a sinister lesion were found it would have been difficult to conduct full clearance.
The patient had CT scans conducted that showed erosive processes around the intermediate and lateral cuneiforms extending into the plantar aspect (Fig. 2). These appearances were similar to the previous MRI taken 8 months ago. It was felt this could be due to joint-based erosive chronic inflammation and atypical infection such as TB. However, the patient had no TB symptoms and a recent negative Heaf test.
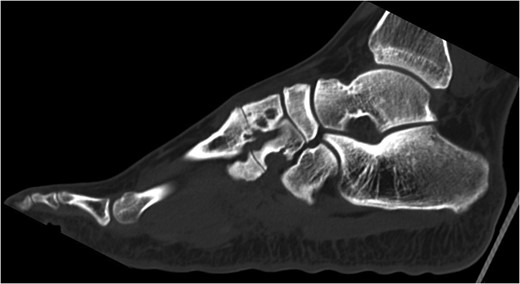
CT scan of left foot. Erosive bony changes are visible of the intermediate and lateral cuneiforms and the corresponding metacarpal bases. These erosions vary in size from 5 to 7 mm.
The patient had an magnetic resonance (MR) angiogram and Doppler US to investigate the lesion further. MR angiogram demonstrated high signal in the intermediate and lateral cuneiform bones in keeping with vascular malformation (Fig. 3). US confirmed an abnormal communication between metatarsal artery and vein at sites in foot where he experienced most pain. These images were discussed at a joint vascular and plastics MDT where a diagnosis of an AVM was concluded.
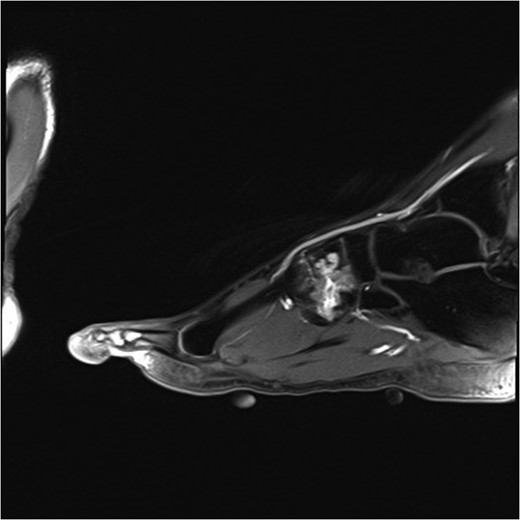
MRI angiogram of left foot. High signal in the midfoot bone around the intermediate and lateral cuneiform bones in keeping with a venous malformation.
Our patient underwent sclerotherapy and under US guidance the nidus of the venous malformation was accessed and 1 ml of 1% sclerosant was injected. A compression bandage was applied post-operatively and 1 month later he reported marked improvement in symptoms.
Discussion
AVMs are congenital vascular lesions resulting from abnormal morphogenesis in early intrauterine life. Other less common causes include trauma, degenerative vascular diseases and iatrogenic sources. Most commonly AVMs affect the pelvis and intracranial circulation with few reports in the foot [2].
In AVMs there is a central body or nidus with no intervening capillary bed, which leads to low vascular resistance within the lesion [2]. Most are subclinical but when symptomatic can have detrimental effects on surrounding soft tissues and cause erosive bone effects from the altered blood flow [3].
Although rarely reported in the foot they should be included when considering differential diagnosis for foot pain. Since most orthopaedic surgeons will rarely encounter routine AVMs, they are often missed in the differential list and can be even more ambiguous by non-specific presenting symptoms as in our case [2].
The most defining examination findings are raised temperature, palpable thrill and audible bruit but in cases may not be evident especially if the lesions are intra/juxta osseous [4]. Other common findings include pain, swelling, varices, mass and functional impairment. MRI is an important tool for assessing AVMs with multiple signal voids apparent representing the dysplastic vessels in the centre of the AVM. It is also the most accurate diagnostic tool since it utilizes a gradient echo technique with vascular parameters and can be used in combination with magnetic resonance angiography [5].
Indications for treatment of AVMs include pain, functional impairment, significant deformity, ischaemia, haemorrhage and overload of the cardiovascular system.
Various treatment options exist for AVMs that warrant treatment. Treatment is not straightforward and dependent on the foot's blood supply. Options include ligation, surgical excision, amputation and embolotherapy (Table 1).
| Intervention . | Description . |
|---|---|
| Ligation |
|
| Surgical excision |
|
| Embolotherapy |
|
| Intervention . | Description . |
|---|---|
| Ligation |
|
| Surgical excision |
|
| Embolotherapy |
|
| Intervention . | Description . |
|---|---|
| Ligation |
|
| Surgical excision |
|
| Embolotherapy |
|
| Intervention . | Description . |
|---|---|
| Ligation |
|
| Surgical excision |
|
| Embolotherapy |
|
Conclusion
We have presented an uncommon case of foot AVM with presenting with pain and erosive bony changes. This presentation created a diagnostic dilemma and almost resulted in a biopsy that may have been detrimental.
Given most foot and ankle surgeons rarely encounter AVMs in routine work, it is important that AVM differential is considered in any diagnosis of foot pain. Clinicians should be aware of the history, symptoms and signs of AVMs and consider MRI with or without digital subtraction angiography when suspected.
Acknowledgements
We declare no sources of funding for our work.
Conflict of interest statement
None declared.
References
- congenital arteriovenous malformation
- magnetic resonance imaging
- sclerotherapy
- diagnostic radiologic examination
- ultrasonography
- computed tomography
- magnetic resonance angiography
- physical examination
- angiography, digital subtraction
- bone resorption
- metatarsal bone
- pain
- diagnosis
- foot pain
- bone lesion
- midfoot
- navicular bone of foot
- erosion



