-
PDF
- Split View
-
Views
-
Cite
Cite
Amarvir Bilkhu, Frances Mosley, Jay A. Gokhale, 21st century twist on Cullen's sign: new generation anticoagulants and splenic traum, Journal of Surgical Case Reports, Volume 2016, Issue 8, August 2016, rjw114, https://doi.org/10.1093/jscr/rjw114
Close - Share Icon Share
Abstract
New anticoagulants such as Rivaroxaban have become a popular choice for patients needing anticoagulation for atrial fibrillation or venous thromboembolism, chiefly because anticoagulation is maintained without the need for monitoring. This can be problematic in cases of trauma, and in this article, we discuss the management and outcome of managing an elderly patient with a shattered spleen while on Rivaroxaban.
INTRODUCTION
The new generation oral anticoagulants include the direct thrombin inhibitor, Dabigatran and Factor Xa inhibitors Rivaroxaban and Apixaban. Factor Xa inhibitors are now widely used for stroke prevention in atrial fibrillation (AF) and in the treatment and prevention of venous thromboembolism (VTE). A major benefit of these agents, over the Vitamin K antagonist, Warfarin, is that they do not require serial monitoring. A recent meta-analysis has shown Rivaroxaban to be a safe alternative to warfarin with significantly lower rates of intracranial bleeding and fatal haemorrhage risk, while also achieving improved efficacy in stroke prevention [1].
The main disadvantage of these drugs is lack of a direct reversing agent which can cause significant problems in the setting of trauma and emergency surgery. Although Dabigatran can be reversed by haemodialysis, this method is ineffective for the Factor Xa inhibitors [2].
Vitamin K and freshly frozen plasma (FFP) have limited efficacy in reversing the anticoagulant effect and although the use of Octaplex and Factor VIII inhibiting agents has been advocated in major bleeding, these are expensive and may be potentially difficult to obtain in emergency situations.
Blunt splenic injuries in the adult population can entail significant haemorrhage. However, ~60% are managed conservatively, with a 10% failure rate of this approach [3]. Management of splenic injury in the elderly population may be further complicated by co-morbidity and frailty; despite this there is literature that describes high rates of success when non-operative management was adopted in patients >55 years of age [4].
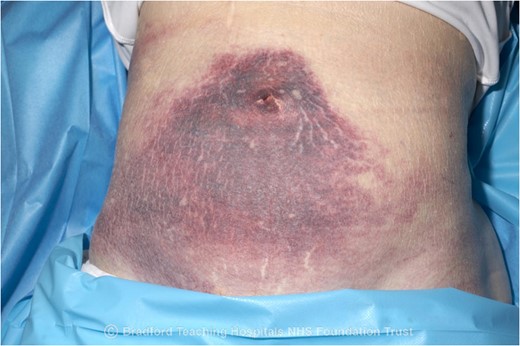
Cullen's sign, first described by Thomas Stephen Cullen in 1916 [5], describes peri-umbilical bruising. Initially reported as a clinical sign in relation to a ruptured ectopic pregnancy, it may be present in many other conditions causing intrabdominal haemorrhage including haemorrhagic pancreatitis, splenic injury and aortic aneurysm rupture. Grey–Turner's sign of bruising in the flanks, indicating retroperitoneal bleeding, may also accompany Cullen's sign.
CASE REPORT
An 80-year-old female was admitted to the acute elderly care team with acute confusion and syncope resulting in a fall. Her past medical history consisted of atrial fibrillation (AF), mitral regurgitation and osteoporosis; and she was anti-coagulated on Rivaroxaban. Prior to the fall, she experienced re-syncopal symptoms of dizziness and vertigo. Her regular medications included Digoxin, Bumetanide and Nebivolol.
On initial presentation, she was stable from a cardiovascular perspective and there were no signs of peritonitis. However, there was tenderness in the left upper abdomen and thorax. An erect chest radiograph showed a left lower pneumonia only. Her blood investigations demonstrated a haemoglobin level of 96 g/L, a platelet count of 230 000/μL and an elevated prothrombin time of 22 s in keeping with her anticoagulation.
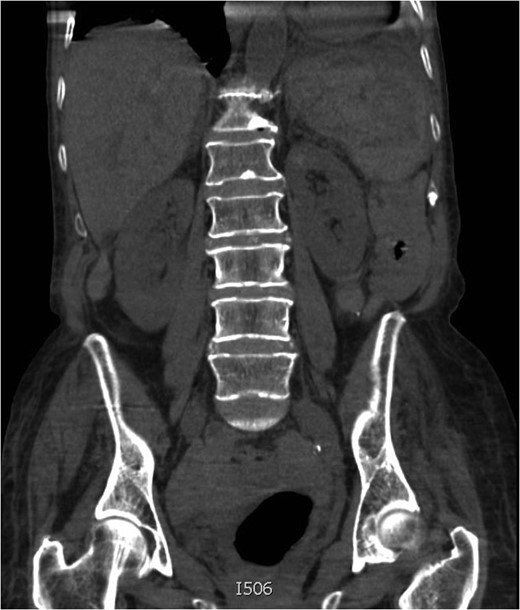
On Day 4, her haemoglobin had decreased to 64 g/dL. Her blood pressure and heart rate remained within normal parameters but a repeat clinical examination revealed a large peri-umbilical ecchymosis (Cullen's sign) (Figs 1 and 2). At this point, she was referred to the surgical team and a computed tomography (CT) scan confirmed a grade V splenic injury with overlying rib fractures, free fluid within the pelvis, but no active bleeding (Figs 3 and 4). The patient's Rivaroxaban was discontinued and Haematology advice was sought. The patient was transfused with packed red blood cells and managed non-operatively. The patient responded well to fluid and blood-product resuscitation, and since discussion with the Radiology team excluded active haemorrhage on the CT non-operative treatment was opted. Concurrent treatment was given for pneumonia and the patient was discharged on the 14th day. Rivaroxaban was re-commenced in the community on discharge following advice from the hospital Haematology team. A 24-h ECG and cardiology follow-up was arranged as an outpatient. Up to the current time of publication, her recovery has been unremarkable.


DISCUSSION
Admissions secondary to falls in the elderly are incredibly common and these patients may not always be considered as classical ‘trauma’ patients. As a significant proportion of elderly patients will be anti-coagulated, they are at increased risk of haemorrhagic complications of injuries sustained. It should also be borne in mind that many of those anti-coagulated for AF may also be on rate-controlling medications, such as beta-adrenoceptor-blocking agents, which may mask the early clinical signs of haemorrhage. For these reasons, these patients with a history of a low-impact fall and falsely reassuring clinical parameters may lead to a late radiographic diagnosis of an acute intra-abdominal injury.
There should be a high index of suspicion when assessing patients such as this, in particular, where a decision regarding anticoagulation needs to be made. Early imaging will identify significant injuries and allows optimization of medical treatment, which will improve survival in these high-risk patients. Although ultrasound and focused assessment with sonography for trauma (FAST) scanning in the Emergency Department may be effective at detecting free intra-peritoneal fluid keeping with likely solid organ injury, CT radiography with intravenous contrast serves as a more sensitive and specific modality for confirming and identifying the grade of splenic injury, as well as helping to diagnose active haemorrhage. A negative FAST examination is not satisfactory in excluding splenic injury. Given the choice in an unstable patient, CT scanning may well be a more timely and useful option for diagnosis before possibly proceeding to a laparotomy.
Regarding the novel anticoagulants in use today, research into reversal strategies is ongoing and as such we would recommend early involvement of a haematologist to assist with these patients; whether they need surgery or not.
CONFLICT OF INTEREST STATEMENT
None declared.



