-
PDF
- Split View
-
Views
-
Cite
Cite
Tomofumi Takenaka, Yu-ichiro Ohnishi, Satoru Oshino, A case of T2 radiculopathy after anterior C5–6 fusion, Journal of Surgical Case Reports, Volume 2016, Issue 5, May 2016, rjw098, https://doi.org/10.1093/jscr/rjw098
Close - Share Icon Share
Abstract
Thoracic radiculopathy is a rare entity. Symptomatic adjacent-segment disease after anterior cervical fusion occurs commonly in the lower cervical spine segment. We describe the clinical presentation and treatment of T2 radiculopathy after C5–6 anterior fusion. A 60-year-old man presented with the right axillary pain for 3 months. He had undergone C5–6 anterior fusion for cervical spondylosis 5 years prior. Computed tomography (CT) and magnetic resonance images showed T2–3 degenerative disease. C5–6 anterior fusion exacerbated the T2–3 segment involved in the patient’s scoliotic deformity. After 2 months of conservative treatment, we decompressed the T2 foramen via T2–3 hemilaminectomy and partial facet resection. After the surgery, his symptoms disappeared. T2 radiculopathy is rare but should be considered in the differential diagnosis of chest pain. Surgeons should pay attention not only to adjacent-segment disease but also to segmental degeneration at the apex of a scoliotic deformity after cervical anterior fusion.
Introduction
The thoracic spine is mechanically stabilized by the rib heads and facet joints. Therefore, thoracic radiculopathy due to degenerative root canal stenosis is a rare entity. Here, we present a patient with right T2 nerve root canal stenosis with pain in the right axilla and posteromedial arm. He had undergone C5–6 anterior fusion for cervical spondylosis 5 years prior. C5–6 anterior fusion exacerbated the T2–3 segment involved in the patient’s scoliotic deformity.
Case Report
A 60-year-old man presented with 3 months of progressive pain in the right axilla and posteromedial upper extremity. He had undergone C5–6 anterior fusion for cervical spondylosis 5 years prior (Fig. 1B). He had returned to his job as a taxi driver after the anterior fusion. He did not have any traumatic injury or traffic accidents after his anterior fusion. His numerical pain scale rating was 10/10. Examination revealed no sensory disturbance, no abnormal tendon-jerk reflexes and progression of muscle weakness. Cervicothoracic scoliosis had been diagnosed before his anterior cervical fusion (Fig. 1A). Roentgenograms showed scoliosis with a right cervicothoracic curvature with a Cobb angle of 17 degrees before his anterior fusion (Fig. 1A) and 19 degrees on referral to our hospital (Fig. 1B). In addition, computed tomography (CT) scanning revealed bone spurs of the C6–7 facets (Fig. 2F). Magnetic resonance (MR) imaging showed a decrease in intervertebral height, but the nerve root canal was preserved at the C6–7 level. CT images also showed osteophytes of the superior costal facet and articular process at the T2–3 level (Fig. 2B–D). MR images demonstrated a protruded disc at the T2–3 level (Fig. 2E and F).
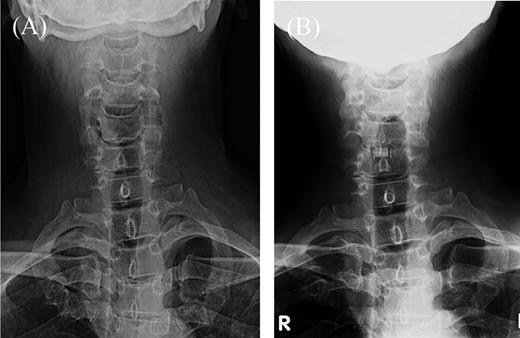
Roentgenograms of C5–6 anterior fusion and scoliosis of the cervicothoracic spine. (A) Cervical frontal view before anterior fusion. (B) Cervical frontal view 5 years after anterior fusion. R: right.
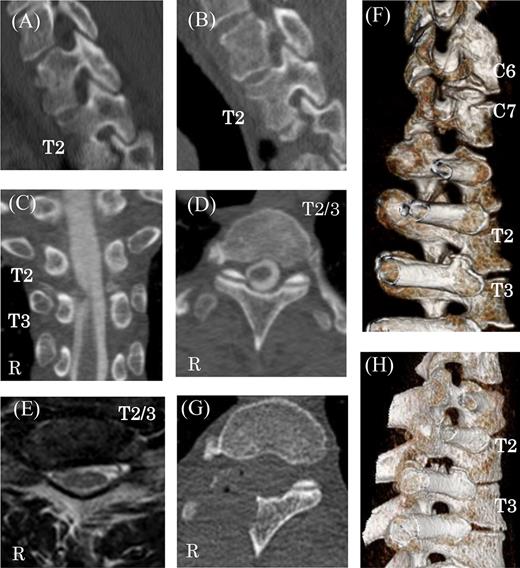
Preoperative and postoperative CT and MR images. (A) Thoracic sagittal views of CT image before cervical anterior fusion at right T2 nerve root canals. Preoperative multi-planar CT images (B–D) and reconstructed 3D images showing right C6–7 and T2–3 nerve root canal stenosis caused by bone spurs of facets and vertebral bodies (F and H). MR imaging of protruded disks at the T2–3 level (E). Postoperative CT shows the decompression of the right T2–3 thoracic nerve root canal (G).
The width and height of the nerve root canal on the right measured 6.4 mm and 4.2 mm at C7 and 5.2 mm and 5.1 mm at T2, respectively [1]. The right C7 and T2 nerve root canals were narrow compared to left side (left C7 width 8.0 mm, height 8.2 mm; left T2 width 9.9 mm, height 10.5 mm). From C5−T4, mean width was 9.4 ± 1.8 mm and mean height was 9.2 ± 2.4 mm. Before anterior cervical fusion, the width and height of the nerve root canal on the right at T2 had been 7.4 mm and 5.0 mm and on the left had been 8.6 mm and 12.2 mm, respectively (Fig. 2A). These findings indicate that the nerve root canals on the right at C7 and T2 were degenerative.
Blood tests, electrocardiogram, electromyogram, somatosensory evoked potential (SSEP) and head MR imaging were all normal. These data provided no evidence of intracranial, peripheral nerve or coronary artery disease. This patient displayed no C7 radiculopathy and had neither delay nor disappearance of SSEP in the median nerve distribution. We therefore diagnosed his symptoms as T2 radicular pain secondary to T2–3 foraminal stenosis. There was no improvement for 2 months with conservative medical treatments.
We performed right T2–3 hemilaminectomy and partial facet resection. After the surgery, his symptoms were remarkably improved. Postoperative CT imaging showed decompression of the T2–3 thoracic nerve root canal (Fig. 2G and H). Six months later, his pain had completely disappeared.
Discussion
Symptomatic thoracic spinal root canal stenosis is regarded as a rare entity. The causes of thoracic radiculopathy include bulging disc, herniated disc, bone spur, spinal canal stenosis or foraminal stenosis. In this patient, osteophytes of the intervertebral joint and the superior costal facet at T2–3, and a bulging disc on the right at T2–3 caused right T2 foraminal stenosis.
Asymmetric bone degeneration, such as disc-endplate degeneration, plays a biomechanical role in the progression of scoliosis [2]. It has been commonly suggested that a spine with scoliosis bears a greater load on the concave side and that this asymmetrical loading causes asymmetrical growth and progression of the deformity [3,4], and has been also suggested that the risk of curve progression is Cobb angle >30 degrees [5], not simply advancing age [6].
Adjacent-segment disease after cervical spine arthrodesis sometimes occurs at the high thoracic levels [7,8], generally occurring in the segment adjacent to the spinal fusion, not in a remote segment. In this case, the patient had undergone C5–6 anterior fusion 5 years prior to presentation. His cervicothoracic scoliosis was diagnosed before his anterior fusion, but curvature was mild. After the cervical anterior fusion, cervicothoracic scoliosis, osteophytes and disc degeneration had been exacerbated. These findings suggest that the mechanical stress after C5–6 anterior fusion burdened not only the adjacent C6–7 segment but also the right T2–3 segment at the apex of the scoliotic curve on the concave side. Degenerative changes occurred at T2–3, which was likely subjected to mechanical stress under asymmetrical loading for 5 years after surgery, resulting in asymmetrical growth and progression of deformity.
We considered cervical angina in this patient’s differential diagnosis due to adjacent-segment degeneration after C5–6 anterior fusion. Walter et al. described the clinical characteristics of cervical angina: a history of cervical radiculopathy, neck pain or pain induced by cervical range of motion [9,10]. In this case, neurological examination showed no C7 segmental or radicular signs. SSEP was also normal. The T2 nerve roots innervate the upper chest, axilla and posteromedial upper extremity areas [10], which correlated anatomically with symptoms in this case. However, a C7 nerve root block could have been performed prior to surgery to further clarify the differential diagnosis.
We report a case of symptomatic T2–3 foraminal stenosis after anterior C5–6 fusion surgery. T2 radiculopathy is rare but should be considered in the differential diagnosis of chest pain, when cardiac ischemia or cervical angina have been ruled out. Surgeons should pay attention not only to adjacent-segment disease but also to segmental degeneration at the apex of a scoliotic deformity after cervical anterior fusion.
Conflict of Interest Statement
None declared.
References
- magnetic resonance imaging
- chest pain
- computed tomography
- cervical spine diseases
- axilla
- differential diagnosis
- pain
- radiculopathy
- surgical procedures, operative
- surgery specialty
- cervical spine
- hemilaminectomy
- tissue degeneration
- conservative treatment
- symptom aggravating factors
- degenerative disorders
- transverse spin relaxation time



