-
PDF
- Split View
-
Views
-
Cite
Cite
Hani B Abdul-Jabar, Jagmeet Bhamra, Tom J Quick, Michael Fox, Iatrogenic posterior tibial nerve division during a combined anterior ankle arthroscopy with an additional posterolateral portal, Journal of Surgical Case Reports, Volume 2016, Issue 5, May 2016, rjw097, https://doi.org/10.1093/jscr/rjw097
Close - Share Icon Share
Abstract
Ankle arthroscopy is an important diagnostic and therapeutic technique in the management of ankle disorders. Nowadays ankle arthroscopy provides good to excellent results (up to 90%) in the treatment of certain intra-articular disorders. Due to the superficial location of ankle joint and the abundance of overlying neurovascular structures, complications reported in ankle arthroscopy are greater than those reported in other joints. We present the first reported case of a complete division of the posterior tibial nerve during an anterior ankle arthroscopy combined with an additional posterolateral portal. This was due to a poorly controlled use of the arthroscopic instruments.
Introduction
Ankle arthroscopy is an important diagnostic and therapeutic technique in the management of ankle disorders. The standard method of ankle arthroscopy was initially described by Takagi in 1939 [1]. In 1972, Watanabe reported on 28 ankle arthroscopies, including a detailed discussion of anteromedial, anterolateral and posterior arthroscopic approaches to the ankle [2].
Nowadays ankle arthroscopy provides good to excellent results (up to 90%) in the treatment of certain intra-articular disorders: the origin of which may be congenital, degenerative, inflammatory or neoplastic [3].
Due to the superficial location of ankle joint and the abundance of overlying neurovascular structures, complications reported in ankle arthroscopy are greater than those reported in other joints [4]. The overall complication rate of ankle arthroscopy is 9%, nearly half of which is attributed to nerve injury [5]. These injuries have been either the direct result of a distractor pin or secondary to incorrect portal placement [6, 7]. To minimize the likelihood of these devastating injuries, surface anatomical landmarks are usually delineated prior to portal placement [6].
In a standard anterior ankle arthroscopy, an anteromedial and anterolateral portals are used. Treatment of combined anterior and posterior ankle pathology usually requires either a combined anterior and posterior arthrotomies or anterior ankle arthroscopy with an additional posterolateral portal. The first technique bears the risk of complications associated with extensive exposure while the latter provides limited access to the posterior ankle joint [8].
The conventional posterolateral portal passes between the Achilles tendon and the sural nerve, approximately 1.2 cm above the tip of the fibula. Both the sural nerve and the small saphenous vein branches must be avoided through this approach. If utilized, the posteromedial portal has predictable risks as it passes between the Achilles tendon and adjacent tibial nerve as part of the neighbouring posterior neurovascular structures [9, 10].
Case Report
The patient was an 18-year-old female who had a congenital talocalcaneal coalition that remained asymptomatic until she reached skeletal maturity. Her symptoms worsened suddenly in the form of severe pain, even at rest and a marked lack of endurance for activity. She also experienced intermittent muscle spasm with an inability to supinate the foot, needing to walk in an adapted position to allow continued ambulation.
She had an arthroscopic debridement and resection of the coalition in October 2008 through a combined anterior ankle arthroscopy with an additional posterolateral portal. She developed progressive pain in the sole of the foot accompanied by localized point tenderness posterior to the medial malleolus with an overlying radiating Tinel’s. She had reduced sensation over the sole of the foot especially for light touch with a very subtle preservation for pin prick particularly over the territory of the medial plantar division.
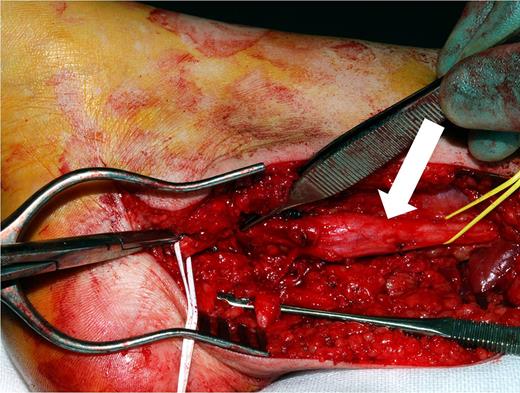
In July 2010, she underwent exploration of her right posterior tibial nerve which revealed its complete division proximal to the bifurcation into the plantar nerves (Fig. 1), and a large (7.2 × 1.2 cm) (Fig. 2) neuroma involving the proximal stump. The distal stump was adherent to the medial capsule by extensive scar tissue. After careful neurolysis and excision of the neuroma, the posterior tibial nerve was reconstructed with three ipsilateral sural nerve cable grafts using Tissel glue.

Complete division of the posterior tibial nerve proximal to the bifurcation into the plantar nerves.
The reconstruction was performed with the ankle in neutral position. After-care consisted of non-weight baring cast immobilization for 4 weeks in approximately 15° of plantar flexion followed by progressive weight baring and full range of motion exercises.
Immediately after surgery, the patient noted a significant reduction in pain attributable to the large neuroma. The remaining sole numbness gradually disappeared over the next several months. She experienced no phantom-like pain in the distribution of the donor sural nerve and had not noticed the sensory loss expected secondary to its grafting.
Three months after surgery, a Tinel sign of equal intensity was present along the course of the nerve reconstruction with early signs of progression. Sequential six monthly follow-ups from then onwards confirmed the distal progression of her Tinel’s with gradual return of normal sensation to the sole of the foot.
Discussion
Neurological complications as a result of ankle arthroscopy have been well documented in the orthopaedic and podiatric literature, but the majority of these did resolve in less than 6 months [6]. All these neurological complications have resulted from inappropriate portal or distractor pin placement, prolonged distraction or the use of a tourniquet. Multiple attempts at portal placement especially if no protective cannula is used can also result in increased soft tissue damage and a subsequent increased risk of subcutaneous nerve and vessel injury.
The exact manoeuvre responsible for dividing the nerve in this case through an anteromedial, anterolateral and posterolateral portals is still not known. The inattentive use of arthroscopic motorized equipment for the talocalcaneal coalition resection is the most likely cause. This equipment can be quite aggressive and may result in violation of the joint capsule and inadvertent damage to the overlying neurovascular structures. Good visualization of the operative field to facilitate debridement and removal of loose bodies requires a delicate balance between inflow, outflow, intra-articular bleeding and instruments manipulation, which may also prove challenging.
Though vigilant attention to the surface anatomy and technique is critical in avoiding the majority neurovascular complications encountered in ankle arthroscopy, our case highlights the importance of adequate visualization, meticulous haemostasis and delicate control of the arthroscopic motorized equipment. Of the several potential complications, injury to the posterior tibial nerve is the most overwhelming.
Conflict of Interest Statement
None declared.



