-
PDF
- Split View
-
Views
-
Cite
Cite
Georgios Sahsamanis, Panagiotis Triantafylakis, Konstantinos Gkouzis, Konstantinos Katis, Georgios Dimitrakopoulos, Intra-abdominal myositis ossificans in an asymptomatic patient during closure of a Hartmann's colostomy, Journal of Surgical Case Reports, Volume 2016, Issue 11, November 2016, rjw203, https://doi.org/10.1093/jscr/rjw203
Close - Share Icon Share
Abstract
Intra-abdominal myositis ossificans, also known as heterotopic mesenteric ossification, defines the formation of bone-like lesions inside the abdominal cavity. It is a rare medical condition, usually following abdominal surgery or trauma. A 55-year-old male presented for closure of a Hartmann's colostomy, created 6 months ago because of sigmoid adenocarcinoma. Intraoperative findings consisted of an elongated bone-like lesion attached on the peritoneum and protruding inside the abdominal cavity, while two more stiff calcified nodules were found in the mesocolon. All lesions were excised. The presence of a hard consistency sigmoid stump led to cancelation of the operation. Heterotopous bone formation constitutes a challenging surgical condition, since its clinical presentation is innocuous and repetitive surgery acts a stimuli for additional bone creation. Computed tomography scan plays a major role in its diagnosis, while nonsteroidal anti-inflammatory drugs and cimetidine are helpful in preventing further recurrence of the disease.
INTRODUCTION
Heterotopic mesenteric ossification (HMO) refers to the formation of bone-like lesions in abnormal locations inside the abdominal cavity. It is a rare disorder with innocuous manifestation, developing after abdominal surgery or trauma. Various imaging modalities are implemented in order to identify and locate the heterotopous bone formations, with computed tomography (CT) scan being the method of choice. Treatment of HMO poses a challenge, since repetitive operations act as a stimulus for the development of further and more aggressive heterotopous bone formations. We present the case of an asymptomatic 55-year-old male with heterotopous intra-abdominal bone-like lesions found during closure of a Hartmann's colostomy.
CASE REPORT
A 55-year-old male presented in our surgical department regarding closure of a Hartmann's colostomy, created 6 months ago because of sigmoid adenocarcinoma. He was symptom free while having the colostomy, with his medical history including hypertension and glaucoma. Preoperative workup was unremarkable, with normal laboratory examination results, and an unremarkable chest radiograph. After written consent, the patient was taken to the operating room.
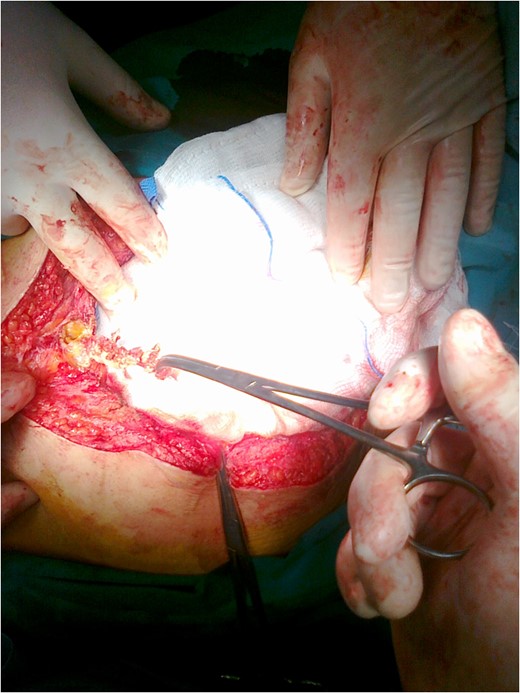
Excision of an elongated bone-like lesion located in the lower abdomen, attached on the peritoneum.

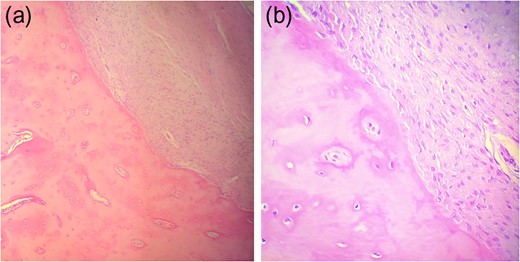
(a, b) Maturation pattern with fibroblastic stroma in association with mature, compact bone and presence of osteoblastic rimming and immature woven bone at the interface between them.
Patient was discharged on the third post-surgical day uneventfully. At 3-month follow-up, he was symptom free, while a CT examination was negative regarding the presence of intra-abdominal bone formations.
DISCUSSION
Heterotopic ossification (HO) describes the formation of bone tissue in extraskeletal nonossifying soft tissue locations. It usually develops in elderly patients following hip surgery or after spinal cord injuries [1, 2]. It is also associated with a rare congenital disease known as fibrodysplasia ossificans progressiva, in which fibrous tissue ossifies spontaneously or post-traumatic [3].
HMO or intra-abdominal myositis ossificans comprises a subgroup of HO, in which a bone-like pseudotumor is formed in the base of the mesentery. Heterotopous bone can also develop in the peritoneum as seen in our case, the mesocolon or adjacent to abdominal surgical incisions [1, 4, 5]. Based on etiology, HMO can be categorized as post-traumatic or post-surgical. Post-traumatic HMO is described after abdominal blunt or stab wounds or gunshots, while post-surgical ossification develops after abdominal surgery.
The development of mesentery ossification shows a preference in middle-age male population with a men to women ratio of 1.5:1 [6]. Occurrence is reported weeks to years after abdominal surgery or trauma [7]. Diagnosis of HMO requires a high index of clinical suspicion, since its presentation is ambiguous, with non-specific abdominal symptoms resembling bowel obstruction. Vague abdominal pain, nausea and vomiting are the main complaints, while physical examination is usually unremarkable. Laboratory examinations are within normal limits, with the possibility of elevated alkaline phosphatase values found in some cases. This reflects the increased osteoblastic activity during heterotopous bone formation [6].
Two theories have been described regarding pathogenesis and formation of the heterotopous bone tissue. One is associated with vertical midline incisions, while the second seems to be connected with inflammation stimuli due to abdominal injury. In the first case, damage to the sternum intraoperatively causes periosteum molecules to proliferate and scatter in the abdominal cavity, forming bone tissue. In the second occasion, abdominal trauma or injury stimulates undifferentiated mesenchymal cells in the abdomen to develop into osteoblasts or chondroblasts. In our case, the second theory seems more suitable; the sigmoidectomy performed 6 months ago probably acted as the required stimuli leading to the development of heterotopous bone [8].
There is an assortment of imaging modalities for the diagnosis of HMO. Ultrasonography cannot directly depict bone formations; still it can reveal hyperechoic strands with an acoustic shadow, indicating calcification of the scanned area. Abdominal X-ray can be significant for opacificated areas with mature trabecular textures, while Tc-99m single-photon emission CT is useful for the intra-abdominal identification of bone formations [6, 9]. CT scan is the method of choice regarding diagnosis of HMO, imaging dispersed trabecular and cortical bone-like lesions in the mesentery, omentum or near the surgical incision [10]. Differential diagnosis includes calcified abdominal cysts or neoplasms due to dystrophic calcification, extravasations or active bleeding [9, 10].
Treatment of HMO is either medical or surgical, depending on patient's clinical condition and the extension of ossification. Decision-making regarding excision of these lesions is challenging, since heterotopous bone formation is subject to recurrence after repetitive surgery [2]. Bone lesions must be excised in cases which the ossificated areas cause bowel obstruction and abdominal symptoms. There are reports indicating that nonsteroidal anti-inflammatory drugs and cimetidine prevent the recurrence of ossification [2, 6]. In our case, the best course of action was to excise the ossificated formations found in the mesocolon and the abdominal trauma. Closure of Hartman's colostomy was avoided, since palpation of the sigmoid stump indicated the presence of bone tissue, putting a possible anastomosis in danger. In conclusion, the ambiguous presentation along with its rarity and recurrent development after repetitive surgery renders treatment of heterotopous mesenteric ossification challenging and demanding. Therapeutic plan must be individually tailored, depending on patient's clinical condition and extend of ossification. Surgical therapy must be reserved for patients experiencing bowel obstruction symptoms, while asymptomatic patients must be observed with radiological examinations for progression of the disease.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
Nothing to declare.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and corresponding images.
REFERENCES
- cimetidine
- computed tomography
- adenocarcinoma
- amputation stumps
- anti-inflammatory agents, non-steroidal
- intraoperative care
- mesentery
- mesocolon
- myositis ossificans
- osteogenesis
- surgical procedures, operative
- wounds and injuries
- abdomen
- colostomy procedure
- diagnosis
- peritoneum
- abdominal surgery
- Abdominal cavity
- calcified nodule



