-
PDF
- Split View
-
Views
-
Cite
Cite
Priyank Sinha, Sasan Panbehchi, Ming-Te Lee, Tejal Parekh, Debasish Pal, Spontaneous resolution of symptomatic lumbar synovial cyst, Journal of Surgical Case Reports, Volume 2016, Issue 10, October 2016, rjw166, https://doi.org/10.1093/jscr/rjw166
Close - Share Icon Share
Abstract
Lumbar synovial cyst arises from the facet joint and can lead to back pain, radiculopathy, neurogenic claudication or even cauda equina syndrome. Although most surgeons would consider surgery to be the treatment of choice, the natural history of the disease process remains unknown and uncertainty still exists regarding optimal management of this controversial entity. We illustrate a case of large L5/S1 synovial cyst for which surgery was initially planned. However, it resolved spontaneously without any treatment. We also provide a brief literature review regarding conservative, surgical and minimally invasive management of symptomatic lumbar synovial cyst with special reference to patient outcome.
CLINICAL DETAILS
A 66-year-old male presented to our institution with 12 months history of severe back pain and left leg pain in L5/S1 distribution. On examination he had a normal neurology except for a dull left ankle jerk. Magnetic resonance imaging (MRI) of his lumbo-sacral spine showed a left L5/S1 synovial cyst (Fig. 1a and b). The findings and management options were discussed with the patient, who decided for a surgical option. However in view of his recent cardiac history it was decided to see him again in clinic in 6 months’ time. After reviewing him in clinic, he was added to the surgical waiting list and as his MRI scan was a year old, fresh set of scans was requested nearer to his operation date. Surprisingly his repeat MRI showed complete resolution of the L5/S1 synovial cyst (Fig. 2a and b).
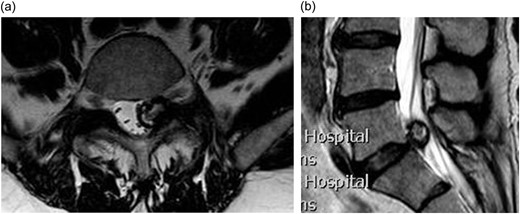
(a) Axial T2 weighted MRI showing a left sided L5/S1 synovial cyst impinging on the left S1 nerve root; (b) sagittal T2 weighted MRI showing a L5/S1 synovial cyst.
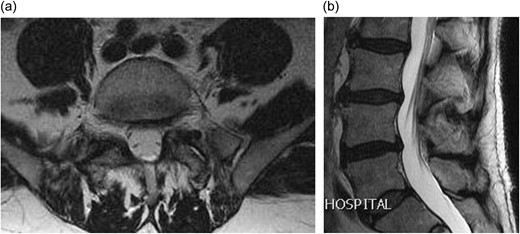
(a) Axial T2 weighted MRI showing complete resolution of the synovial cyst; (b) sagittal T2 weighted MRI showing complete resolution of the synovial cyst.
DISCUSSION
Synovial cyst is a cyst with clear or xanthochromic fluid within a synovium lined cavity which communicates with a joint capsule [1]. In the lumbar spine, synovial cyst arises from the medial margin of the facet joint and can cause lateral recess or central canal stenosis leading to radiculopathy, neurogenic claudication, sensory or motor deficits, reflex abnormalities and back pain [2]. At times it may be asymptomatic and discovered incidentally.
Synovial cysts are most common in the sixth decade of life as seen in our patient. Though our patient was a male, synovial cyst may have a slight female preponderance and most common spinal level affected is L4–L5 followed by L5–S1, L3–L4 and L2–L3 [3]. Incidence of lumbar synovial cyst (LSC) ranges between 0.8% and 2.0% on imaging [4] whereas it is between 0.01% and 0.8% [4] among patients undergoing lumbar spinal surgery. However, the exact etiopathogenesis of these synovial cysts is unclear but factors such as facet joint arthropathy, spinal instability and degenerative spondylolisthesis causing micro-trauma have been implicated [3].
MRI is the modality of choice for diagnosing synovial cysts as sensitivity of computer tomography (CT) is only 60% as compared to 90–95% for MRI [5, 6]. MRI appearance depends upon the composition of the cystic fluid. MRI typically shows a well-defined extra-dural mass with iso-intense fluid signal on T1 and hyper-intense fluid signal on T2 [1]. Hyper-intensity on T1 may indicate the presence of high protein content or hemorrhage whereas hypo-intensity on both T1 and T2 sequences indicate the presence of calcification.
Management of symptomatic LSC is controversial as natural history of the disease is unknown. Treatment options are conservative and surgical. Conservative management includes bed rest, analgesia, bracing, CT guided percutaneous cyst aspiration and facet joint and epidural steroid injection. A number of authors have published results of conservative management with varying degree of success (Table 1). Surgery is indicated in patients with progressive neurological deficit or intractable pain not responding to conservative treatment. However, there is also controversy regarding ideal surgical management. Some surgeons recommend cyst excision with decompression as a primary procedure whereas others tend to combine it with spinal fusion as degenerative spondylolisthesis can be present in a number of patients with LSC (38.0–75.0%) [6] (Table 2). Though there is no consensus regarding management of degenerative spondylolisthesis associated with LSC. Some authors [7] advocate fusion as a primary procedure in the presence of instability or when facetectomy is performed for the management of LSC whereas others [8] recommend pre- and post-operative dynamic studies to assess suitability for fusion either as a primary or secondary procedure.
Case series describing conservative management of symptomatic LSC in literature
| Author . | Journal . | No of patients . | Treatment modality . | Procedure . | Outcome . |
|---|---|---|---|---|---|
| Marthaet al., 2009 | The Spine Journal | 101 | Conservative | Facet joint injection and attempted cyst rupture | Pre-procedure mean* back pain, leg pain and Oswestry Disability Index were 5.5, 7.4 and 46.4. Post-procedure mean back pain, leg pain and Oswestry Disability Index were 2.3, 2.1 and 19.4. 55 patients later required surgery |
| Cyst ruptured in 81 patients | |||||
| *On numeric rating scale | |||||
| Allen et al., 2009 | The Spine Journal | 32 | Conservative | Percutaneous cyst rupture + transforaminal epidural steroid injection + facet joint injection – 17 | Excellent – 23 |
| Percutaneous cyst rupture + facet joint injection – 15 | *Twelve patients had synovial cyst recurrence of which five had complete resolution of symptoms after repeat rupture, whereas six underwent surgery for the removal of the cyst | ||||
| Sabers et al., 2005 | Archives of physical medicine and rehabilitation | 18 | Conservative | Cyst aspiration + facet joint injection + transforaminal epidural steroid injection | Long-term pain relief – 9 |
| *Nine later required surgery | |||||
| Shah and Lutz, 2003 | The Spine Journal | 10 | Conservative | cyst aspiration + transforaminal epidural steroid injection – 5 | Symptoms improved – 1 |
| cyst aspiration + steroid instillation – 5 | *Eight later required surgery for pain relief | ||||
| Bureau et al., 2001 | Radiology | 12 | Conservative | Facet joint injection and attempted cyst rupture | Excellent – 9 (six had successful cyst rupture) |
| *Three later underwent surgery | |||||
| Slipman et al., 2000 | Archives of physical medicine and rehabilitation | 14 | Conservative | Selective nerve root block +/– facet joint injection +/– cyst puncture | Excellent – 4 |
| *Seven later required surgery for pain relief | |||||
| Parlier- Cuau et al., 1999 | Radiology | 30 | Conservative | Facet joint injection | Excellent –10 |
| Fair/Poor – 18. Fourteen of these patients later opted for surgery | |||||
| *Two patients were lost to follow-up | |||||
| Hsu et al., 1995 | Spine | 19 | Conservative | Epidural steroid injection – 4 | Epidural steroid injection provided significant pain relief in three patients lasting from 3 weeks to 2 months whereas facet joint injection resulted in good, partial and no pain relief in one patient each. |
| Facet Joint injection – 3 | |||||
| *Six patients improved with rest, medications and bracing only. Three patients were not treated as the cyst was an incidental finding and two patients were not included in follow-up. Eight patients later required surgery |
| Author . | Journal . | No of patients . | Treatment modality . | Procedure . | Outcome . |
|---|---|---|---|---|---|
| Marthaet al., 2009 | The Spine Journal | 101 | Conservative | Facet joint injection and attempted cyst rupture | Pre-procedure mean* back pain, leg pain and Oswestry Disability Index were 5.5, 7.4 and 46.4. Post-procedure mean back pain, leg pain and Oswestry Disability Index were 2.3, 2.1 and 19.4. 55 patients later required surgery |
| Cyst ruptured in 81 patients | |||||
| *On numeric rating scale | |||||
| Allen et al., 2009 | The Spine Journal | 32 | Conservative | Percutaneous cyst rupture + transforaminal epidural steroid injection + facet joint injection – 17 | Excellent – 23 |
| Percutaneous cyst rupture + facet joint injection – 15 | *Twelve patients had synovial cyst recurrence of which five had complete resolution of symptoms after repeat rupture, whereas six underwent surgery for the removal of the cyst | ||||
| Sabers et al., 2005 | Archives of physical medicine and rehabilitation | 18 | Conservative | Cyst aspiration + facet joint injection + transforaminal epidural steroid injection | Long-term pain relief – 9 |
| *Nine later required surgery | |||||
| Shah and Lutz, 2003 | The Spine Journal | 10 | Conservative | cyst aspiration + transforaminal epidural steroid injection – 5 | Symptoms improved – 1 |
| cyst aspiration + steroid instillation – 5 | *Eight later required surgery for pain relief | ||||
| Bureau et al., 2001 | Radiology | 12 | Conservative | Facet joint injection and attempted cyst rupture | Excellent – 9 (six had successful cyst rupture) |
| *Three later underwent surgery | |||||
| Slipman et al., 2000 | Archives of physical medicine and rehabilitation | 14 | Conservative | Selective nerve root block +/– facet joint injection +/– cyst puncture | Excellent – 4 |
| *Seven later required surgery for pain relief | |||||
| Parlier- Cuau et al., 1999 | Radiology | 30 | Conservative | Facet joint injection | Excellent –10 |
| Fair/Poor – 18. Fourteen of these patients later opted for surgery | |||||
| *Two patients were lost to follow-up | |||||
| Hsu et al., 1995 | Spine | 19 | Conservative | Epidural steroid injection – 4 | Epidural steroid injection provided significant pain relief in three patients lasting from 3 weeks to 2 months whereas facet joint injection resulted in good, partial and no pain relief in one patient each. |
| Facet Joint injection – 3 | |||||
| *Six patients improved with rest, medications and bracing only. Three patients were not treated as the cyst was an incidental finding and two patients were not included in follow-up. Eight patients later required surgery |
Case series describing conservative management of symptomatic LSC in literature
| Author . | Journal . | No of patients . | Treatment modality . | Procedure . | Outcome . |
|---|---|---|---|---|---|
| Marthaet al., 2009 | The Spine Journal | 101 | Conservative | Facet joint injection and attempted cyst rupture | Pre-procedure mean* back pain, leg pain and Oswestry Disability Index were 5.5, 7.4 and 46.4. Post-procedure mean back pain, leg pain and Oswestry Disability Index were 2.3, 2.1 and 19.4. 55 patients later required surgery |
| Cyst ruptured in 81 patients | |||||
| *On numeric rating scale | |||||
| Allen et al., 2009 | The Spine Journal | 32 | Conservative | Percutaneous cyst rupture + transforaminal epidural steroid injection + facet joint injection – 17 | Excellent – 23 |
| Percutaneous cyst rupture + facet joint injection – 15 | *Twelve patients had synovial cyst recurrence of which five had complete resolution of symptoms after repeat rupture, whereas six underwent surgery for the removal of the cyst | ||||
| Sabers et al., 2005 | Archives of physical medicine and rehabilitation | 18 | Conservative | Cyst aspiration + facet joint injection + transforaminal epidural steroid injection | Long-term pain relief – 9 |
| *Nine later required surgery | |||||
| Shah and Lutz, 2003 | The Spine Journal | 10 | Conservative | cyst aspiration + transforaminal epidural steroid injection – 5 | Symptoms improved – 1 |
| cyst aspiration + steroid instillation – 5 | *Eight later required surgery for pain relief | ||||
| Bureau et al., 2001 | Radiology | 12 | Conservative | Facet joint injection and attempted cyst rupture | Excellent – 9 (six had successful cyst rupture) |
| *Three later underwent surgery | |||||
| Slipman et al., 2000 | Archives of physical medicine and rehabilitation | 14 | Conservative | Selective nerve root block +/– facet joint injection +/– cyst puncture | Excellent – 4 |
| *Seven later required surgery for pain relief | |||||
| Parlier- Cuau et al., 1999 | Radiology | 30 | Conservative | Facet joint injection | Excellent –10 |
| Fair/Poor – 18. Fourteen of these patients later opted for surgery | |||||
| *Two patients were lost to follow-up | |||||
| Hsu et al., 1995 | Spine | 19 | Conservative | Epidural steroid injection – 4 | Epidural steroid injection provided significant pain relief in three patients lasting from 3 weeks to 2 months whereas facet joint injection resulted in good, partial and no pain relief in one patient each. |
| Facet Joint injection – 3 | |||||
| *Six patients improved with rest, medications and bracing only. Three patients were not treated as the cyst was an incidental finding and two patients were not included in follow-up. Eight patients later required surgery |
| Author . | Journal . | No of patients . | Treatment modality . | Procedure . | Outcome . |
|---|---|---|---|---|---|
| Marthaet al., 2009 | The Spine Journal | 101 | Conservative | Facet joint injection and attempted cyst rupture | Pre-procedure mean* back pain, leg pain and Oswestry Disability Index were 5.5, 7.4 and 46.4. Post-procedure mean back pain, leg pain and Oswestry Disability Index were 2.3, 2.1 and 19.4. 55 patients later required surgery |
| Cyst ruptured in 81 patients | |||||
| *On numeric rating scale | |||||
| Allen et al., 2009 | The Spine Journal | 32 | Conservative | Percutaneous cyst rupture + transforaminal epidural steroid injection + facet joint injection – 17 | Excellent – 23 |
| Percutaneous cyst rupture + facet joint injection – 15 | *Twelve patients had synovial cyst recurrence of which five had complete resolution of symptoms after repeat rupture, whereas six underwent surgery for the removal of the cyst | ||||
| Sabers et al., 2005 | Archives of physical medicine and rehabilitation | 18 | Conservative | Cyst aspiration + facet joint injection + transforaminal epidural steroid injection | Long-term pain relief – 9 |
| *Nine later required surgery | |||||
| Shah and Lutz, 2003 | The Spine Journal | 10 | Conservative | cyst aspiration + transforaminal epidural steroid injection – 5 | Symptoms improved – 1 |
| cyst aspiration + steroid instillation – 5 | *Eight later required surgery for pain relief | ||||
| Bureau et al., 2001 | Radiology | 12 | Conservative | Facet joint injection and attempted cyst rupture | Excellent – 9 (six had successful cyst rupture) |
| *Three later underwent surgery | |||||
| Slipman et al., 2000 | Archives of physical medicine and rehabilitation | 14 | Conservative | Selective nerve root block +/– facet joint injection +/– cyst puncture | Excellent – 4 |
| *Seven later required surgery for pain relief | |||||
| Parlier- Cuau et al., 1999 | Radiology | 30 | Conservative | Facet joint injection | Excellent –10 |
| Fair/Poor – 18. Fourteen of these patients later opted for surgery | |||||
| *Two patients were lost to follow-up | |||||
| Hsu et al., 1995 | Spine | 19 | Conservative | Epidural steroid injection – 4 | Epidural steroid injection provided significant pain relief in three patients lasting from 3 weeks to 2 months whereas facet joint injection resulted in good, partial and no pain relief in one patient each. |
| Facet Joint injection – 3 | |||||
| *Six patients improved with rest, medications and bracing only. Three patients were not treated as the cyst was an incidental finding and two patients were not included in follow-up. Eight patients later required surgery |
| Author . | Journal . | No of patients . | Treatment modality . | Procedure . | Outcome . |
|---|---|---|---|---|---|
| Landi et al., 2012 | Neurosurgical review | 15 | Surgery | Cyst excision, hemilaminectomy and medial facetectomy | Complete resolution of symptoms – 12 |
| Improvement in symptoms – 3 | |||||
| Bashir and Ajani, 2012 | World neurosurgery | 21 | Surgery | Cyst excision – 8 | Excellent – 11 |
| Cyst excision + laminectomy – 8 | Good – 5 | ||||
| Cyst excision + laminectomy + fusion – 1 | Fair – 1 | ||||
| *Three patients improved with conservative treatment and 1 patient refused surgery | |||||
| Xu et al., 2010 | Spine | 167 | Surgery | Cyst excision + | Back and radicular pain improved in 91.6% and 91.9% patients |
| facetectomy + instrumented fusion – 56 | |||||
| hemilaminectomy – 51 | *After a mean follow-up of 16 +/– 9 months, 5 patients had recurrent cyst, 36 patients developed recurrent back pain whereas 20 developed recurrent leg pain. | ||||
| bilateral laminectomy – 39 | |||||
| facetectomy + in situ fusion – 18 | |||||
| Boviatsis et al., 2008 | European spine journal | 7 | Surgery | Cyst excision + | Resolution of symptoms – 4 |
| foraminotomy – 3 | Considerable improvement – 3 | ||||
| hemilaminectomy – 2 | |||||
| hemilaminectomy and discectomy – 1 | |||||
| 2 level laminectomy – 1 | |||||
| Weiner et al., 2007 | Journal of orthopaedic surgery and research | 46 | Surgery | Cyst excision + | Resolution of symptoms – 40 |
| *Seven patients later required addition surgery | |||||
| Flavectomy + medial facetectomy + foraminotomy – 23 | |||||
| Flavectomy + medial facetectomy + foraminotomy + fusion – 23 | |||||
| Kusakabe et al., 2006 | Journal of neurosurgery | 45 | Surgery | Cyst excision, flavectomy and medial facetectomy | Resolution of symptoms -45 |
| Metellus et al., 2006 | Acta neurochirurgica | 77 | Surgery | Cyst excision + | Excellent/good – 97.4% |
| partial/total hemilaminectomy proximal foraminotomy and medial facetectomy – 51 | *One patient had cyst recurrence and 1 required fusion for symptomatic spondylolisthesis | ||||
| laminectomy, proximal foraminotomy and medial facetectomy – 26 | |||||
| Khan et al., 2005 | Journal of spinal disorders & techniques | 39 | Surgery | Cyst excision + | Excellent/good – 30 |
| laminectomy + fusion – 26 | Fair/poor – 9 | ||||
| laminectomy – 13 | *Four patients later required fusion procedure whereas 1 patient had cyst recurrence | ||||
| Indar et al., 2004 | Surgeon | 8 | Surgery | Cyst excision, hemilaminotomy, flavectomy and minimal facet joint excision | Excellent – 6 |
| Good – 2 | |||||
| Epstein, 2004 | Spine | 80 | Surgery | Cyst excision + | Excellent/good – 48 |
| Laminectomy + medial facetectomy + foraminotomy – 76 | Fair/poor – 32 | ||||
| Laminectomy + unilateral facetectomy + foraminotomy – 4 | |||||
| *Twelve patients required secondary surgery | |||||
| Pirotte et al., 2003 | Journal of neurosurgery | 46 | Surgery | Cyst excision + | Immediate symptomatic relief was seen in all patients |
| hemilaminectomy – 16 | |||||
| interlaminar decompression – 12 | |||||
| laminectomy – 10 | |||||
| partial hemilaminectomy – 8 | |||||
| Banning et al., 2001 | Spine | 29 | Surgery | Cyst excision and laminotomy was done as primary procedure. | Completely improved – 6 |
| Better – 18 | |||||
| *Two patients later required fusion | |||||
| Two patients also required fusion whereas some others required laminectomy, medial facetectomy and foraminotomy | |||||
| *24/29 response to follow-up | |||||
| Salmon et al., 2001 | Acta neurochirurgica | 28 | Surgery | Cyst excision and medial facetectomy | 26 excellent/good |
| 2 fair/poor | |||||
| Trummer et al., 2001 | Journal of neurology neurosurgery and psychiatry | 19 | Surgery | Cyst excision + | Excellent 17 |
| flavectomy – 8 | Good – 2 | ||||
| hemilaminectomy – 7 | *One patient had cyst recurrence | ||||
| laminectomy – 4 | |||||
| Lyons et al., 2000 | Journal of neurosurgery | 194 | Surgery | Cyst excision –194 + | Good – 134 |
| medial facetectomy – 159 | *47 were lost to follow-up | ||||
| total facetectomy – 23 | *Four patients required delayed fusion for symptomatic spondylolisthesis | ||||
| not specified – 12 | |||||
| + | |||||
| partial hemilaminectomy – 103, | |||||
| total hemilaminectomy/bilateral laminectomy – 86 | |||||
| not specified – 5 | |||||
| 18 patients also had fusion as a primary procedure | |||||
| Howington et al., 1999 | Journal of neurosurgery | 28 | Surgery | Cyst excision + | Resolution of low back pain in 21/26 |
| multilevel laminectomy – 12 | Resolution of leg pain in 19/21 and improved leg pain in 2/21 | ||||
| Partial laminectomy – 10 | |||||
| one-level laminectomy – 5 | |||||
| multilevel laminectomy and in situ fusion – 1 | |||||
| Jonsson et al., 1999 | Acta orthopaedica Scandinavica | 8 | Surgery | Cyst excision + | Excellent –5 |
| foraminotomy – 6 | Good – 3 | ||||
| laminectomy – 2 | |||||
| Sabo et al., 1996 | Journal of neurosurgery | 56 | Surgery | Cyst excision + | Excellent – 40 |
| *60 cysts | medial facetectomy – 55 cysts | Poor – 1 | |||
| medial facetectomy + fusion – 6 | *One patient had cyst recurrence and two patients required delayed fusion for post-operative instability | ||||
| Yarde et al., 1995 | Surgical neurology | 8 | Surgery | Cyst excision + | Dramatic pain improvement was seen in seven patients whereas in one patient symptom resolved after redo surgery for removal of scar tissue. |
| hemilaminectomy – 5 | |||||
| laminectomy – 1 | |||||
| laminectomy + fusion –1 | |||||
| fusion – 1 | |||||
| Freidberg et al., 1994 | Neurosurgery | 23 | Surgery | Cyst excision + | Excellent – 15 |
| Considerable improvement – 7 of which 1 required fusion | |||||
| Poor – 1 | |||||
| hemilaminectomy – 13 | |||||
| Laminectomy – 10 | |||||
| Most patients also underwent partial facetectomy |
| Author . | Journal . | No of patients . | Treatment modality . | Procedure . | Outcome . |
|---|---|---|---|---|---|
| Landi et al., 2012 | Neurosurgical review | 15 | Surgery | Cyst excision, hemilaminectomy and medial facetectomy | Complete resolution of symptoms – 12 |
| Improvement in symptoms – 3 | |||||
| Bashir and Ajani, 2012 | World neurosurgery | 21 | Surgery | Cyst excision – 8 | Excellent – 11 |
| Cyst excision + laminectomy – 8 | Good – 5 | ||||
| Cyst excision + laminectomy + fusion – 1 | Fair – 1 | ||||
| *Three patients improved with conservative treatment and 1 patient refused surgery | |||||
| Xu et al., 2010 | Spine | 167 | Surgery | Cyst excision + | Back and radicular pain improved in 91.6% and 91.9% patients |
| facetectomy + instrumented fusion – 56 | |||||
| hemilaminectomy – 51 | *After a mean follow-up of 16 +/– 9 months, 5 patients had recurrent cyst, 36 patients developed recurrent back pain whereas 20 developed recurrent leg pain. | ||||
| bilateral laminectomy – 39 | |||||
| facetectomy + in situ fusion – 18 | |||||
| Boviatsis et al., 2008 | European spine journal | 7 | Surgery | Cyst excision + | Resolution of symptoms – 4 |
| foraminotomy – 3 | Considerable improvement – 3 | ||||
| hemilaminectomy – 2 | |||||
| hemilaminectomy and discectomy – 1 | |||||
| 2 level laminectomy – 1 | |||||
| Weiner et al., 2007 | Journal of orthopaedic surgery and research | 46 | Surgery | Cyst excision + | Resolution of symptoms – 40 |
| *Seven patients later required addition surgery | |||||
| Flavectomy + medial facetectomy + foraminotomy – 23 | |||||
| Flavectomy + medial facetectomy + foraminotomy + fusion – 23 | |||||
| Kusakabe et al., 2006 | Journal of neurosurgery | 45 | Surgery | Cyst excision, flavectomy and medial facetectomy | Resolution of symptoms -45 |
| Metellus et al., 2006 | Acta neurochirurgica | 77 | Surgery | Cyst excision + | Excellent/good – 97.4% |
| partial/total hemilaminectomy proximal foraminotomy and medial facetectomy – 51 | *One patient had cyst recurrence and 1 required fusion for symptomatic spondylolisthesis | ||||
| laminectomy, proximal foraminotomy and medial facetectomy – 26 | |||||
| Khan et al., 2005 | Journal of spinal disorders & techniques | 39 | Surgery | Cyst excision + | Excellent/good – 30 |
| laminectomy + fusion – 26 | Fair/poor – 9 | ||||
| laminectomy – 13 | *Four patients later required fusion procedure whereas 1 patient had cyst recurrence | ||||
| Indar et al., 2004 | Surgeon | 8 | Surgery | Cyst excision, hemilaminotomy, flavectomy and minimal facet joint excision | Excellent – 6 |
| Good – 2 | |||||
| Epstein, 2004 | Spine | 80 | Surgery | Cyst excision + | Excellent/good – 48 |
| Laminectomy + medial facetectomy + foraminotomy – 76 | Fair/poor – 32 | ||||
| Laminectomy + unilateral facetectomy + foraminotomy – 4 | |||||
| *Twelve patients required secondary surgery | |||||
| Pirotte et al., 2003 | Journal of neurosurgery | 46 | Surgery | Cyst excision + | Immediate symptomatic relief was seen in all patients |
| hemilaminectomy – 16 | |||||
| interlaminar decompression – 12 | |||||
| laminectomy – 10 | |||||
| partial hemilaminectomy – 8 | |||||
| Banning et al., 2001 | Spine | 29 | Surgery | Cyst excision and laminotomy was done as primary procedure. | Completely improved – 6 |
| Better – 18 | |||||
| *Two patients later required fusion | |||||
| Two patients also required fusion whereas some others required laminectomy, medial facetectomy and foraminotomy | |||||
| *24/29 response to follow-up | |||||
| Salmon et al., 2001 | Acta neurochirurgica | 28 | Surgery | Cyst excision and medial facetectomy | 26 excellent/good |
| 2 fair/poor | |||||
| Trummer et al., 2001 | Journal of neurology neurosurgery and psychiatry | 19 | Surgery | Cyst excision + | Excellent 17 |
| flavectomy – 8 | Good – 2 | ||||
| hemilaminectomy – 7 | *One patient had cyst recurrence | ||||
| laminectomy – 4 | |||||
| Lyons et al., 2000 | Journal of neurosurgery | 194 | Surgery | Cyst excision –194 + | Good – 134 |
| medial facetectomy – 159 | *47 were lost to follow-up | ||||
| total facetectomy – 23 | *Four patients required delayed fusion for symptomatic spondylolisthesis | ||||
| not specified – 12 | |||||
| + | |||||
| partial hemilaminectomy – 103, | |||||
| total hemilaminectomy/bilateral laminectomy – 86 | |||||
| not specified – 5 | |||||
| 18 patients also had fusion as a primary procedure | |||||
| Howington et al., 1999 | Journal of neurosurgery | 28 | Surgery | Cyst excision + | Resolution of low back pain in 21/26 |
| multilevel laminectomy – 12 | Resolution of leg pain in 19/21 and improved leg pain in 2/21 | ||||
| Partial laminectomy – 10 | |||||
| one-level laminectomy – 5 | |||||
| multilevel laminectomy and in situ fusion – 1 | |||||
| Jonsson et al., 1999 | Acta orthopaedica Scandinavica | 8 | Surgery | Cyst excision + | Excellent –5 |
| foraminotomy – 6 | Good – 3 | ||||
| laminectomy – 2 | |||||
| Sabo et al., 1996 | Journal of neurosurgery | 56 | Surgery | Cyst excision + | Excellent – 40 |
| *60 cysts | medial facetectomy – 55 cysts | Poor – 1 | |||
| medial facetectomy + fusion – 6 | *One patient had cyst recurrence and two patients required delayed fusion for post-operative instability | ||||
| Yarde et al., 1995 | Surgical neurology | 8 | Surgery | Cyst excision + | Dramatic pain improvement was seen in seven patients whereas in one patient symptom resolved after redo surgery for removal of scar tissue. |
| hemilaminectomy – 5 | |||||
| laminectomy – 1 | |||||
| laminectomy + fusion –1 | |||||
| fusion – 1 | |||||
| Freidberg et al., 1994 | Neurosurgery | 23 | Surgery | Cyst excision + | Excellent – 15 |
| Considerable improvement – 7 of which 1 required fusion | |||||
| Poor – 1 | |||||
| hemilaminectomy – 13 | |||||
| Laminectomy – 10 | |||||
| Most patients also underwent partial facetectomy |
| Author . | Journal . | No of patients . | Treatment modality . | Procedure . | Outcome . |
|---|---|---|---|---|---|
| Landi et al., 2012 | Neurosurgical review | 15 | Surgery | Cyst excision, hemilaminectomy and medial facetectomy | Complete resolution of symptoms – 12 |
| Improvement in symptoms – 3 | |||||
| Bashir and Ajani, 2012 | World neurosurgery | 21 | Surgery | Cyst excision – 8 | Excellent – 11 |
| Cyst excision + laminectomy – 8 | Good – 5 | ||||
| Cyst excision + laminectomy + fusion – 1 | Fair – 1 | ||||
| *Three patients improved with conservative treatment and 1 patient refused surgery | |||||
| Xu et al., 2010 | Spine | 167 | Surgery | Cyst excision + | Back and radicular pain improved in 91.6% and 91.9% patients |
| facetectomy + instrumented fusion – 56 | |||||
| hemilaminectomy – 51 | *After a mean follow-up of 16 +/– 9 months, 5 patients had recurrent cyst, 36 patients developed recurrent back pain whereas 20 developed recurrent leg pain. | ||||
| bilateral laminectomy – 39 | |||||
| facetectomy + in situ fusion – 18 | |||||
| Boviatsis et al., 2008 | European spine journal | 7 | Surgery | Cyst excision + | Resolution of symptoms – 4 |
| foraminotomy – 3 | Considerable improvement – 3 | ||||
| hemilaminectomy – 2 | |||||
| hemilaminectomy and discectomy – 1 | |||||
| 2 level laminectomy – 1 | |||||
| Weiner et al., 2007 | Journal of orthopaedic surgery and research | 46 | Surgery | Cyst excision + | Resolution of symptoms – 40 |
| *Seven patients later required addition surgery | |||||
| Flavectomy + medial facetectomy + foraminotomy – 23 | |||||
| Flavectomy + medial facetectomy + foraminotomy + fusion – 23 | |||||
| Kusakabe et al., 2006 | Journal of neurosurgery | 45 | Surgery | Cyst excision, flavectomy and medial facetectomy | Resolution of symptoms -45 |
| Metellus et al., 2006 | Acta neurochirurgica | 77 | Surgery | Cyst excision + | Excellent/good – 97.4% |
| partial/total hemilaminectomy proximal foraminotomy and medial facetectomy – 51 | *One patient had cyst recurrence and 1 required fusion for symptomatic spondylolisthesis | ||||
| laminectomy, proximal foraminotomy and medial facetectomy – 26 | |||||
| Khan et al., 2005 | Journal of spinal disorders & techniques | 39 | Surgery | Cyst excision + | Excellent/good – 30 |
| laminectomy + fusion – 26 | Fair/poor – 9 | ||||
| laminectomy – 13 | *Four patients later required fusion procedure whereas 1 patient had cyst recurrence | ||||
| Indar et al., 2004 | Surgeon | 8 | Surgery | Cyst excision, hemilaminotomy, flavectomy and minimal facet joint excision | Excellent – 6 |
| Good – 2 | |||||
| Epstein, 2004 | Spine | 80 | Surgery | Cyst excision + | Excellent/good – 48 |
| Laminectomy + medial facetectomy + foraminotomy – 76 | Fair/poor – 32 | ||||
| Laminectomy + unilateral facetectomy + foraminotomy – 4 | |||||
| *Twelve patients required secondary surgery | |||||
| Pirotte et al., 2003 | Journal of neurosurgery | 46 | Surgery | Cyst excision + | Immediate symptomatic relief was seen in all patients |
| hemilaminectomy – 16 | |||||
| interlaminar decompression – 12 | |||||
| laminectomy – 10 | |||||
| partial hemilaminectomy – 8 | |||||
| Banning et al., 2001 | Spine | 29 | Surgery | Cyst excision and laminotomy was done as primary procedure. | Completely improved – 6 |
| Better – 18 | |||||
| *Two patients later required fusion | |||||
| Two patients also required fusion whereas some others required laminectomy, medial facetectomy and foraminotomy | |||||
| *24/29 response to follow-up | |||||
| Salmon et al., 2001 | Acta neurochirurgica | 28 | Surgery | Cyst excision and medial facetectomy | 26 excellent/good |
| 2 fair/poor | |||||
| Trummer et al., 2001 | Journal of neurology neurosurgery and psychiatry | 19 | Surgery | Cyst excision + | Excellent 17 |
| flavectomy – 8 | Good – 2 | ||||
| hemilaminectomy – 7 | *One patient had cyst recurrence | ||||
| laminectomy – 4 | |||||
| Lyons et al., 2000 | Journal of neurosurgery | 194 | Surgery | Cyst excision –194 + | Good – 134 |
| medial facetectomy – 159 | *47 were lost to follow-up | ||||
| total facetectomy – 23 | *Four patients required delayed fusion for symptomatic spondylolisthesis | ||||
| not specified – 12 | |||||
| + | |||||
| partial hemilaminectomy – 103, | |||||
| total hemilaminectomy/bilateral laminectomy – 86 | |||||
| not specified – 5 | |||||
| 18 patients also had fusion as a primary procedure | |||||
| Howington et al., 1999 | Journal of neurosurgery | 28 | Surgery | Cyst excision + | Resolution of low back pain in 21/26 |
| multilevel laminectomy – 12 | Resolution of leg pain in 19/21 and improved leg pain in 2/21 | ||||
| Partial laminectomy – 10 | |||||
| one-level laminectomy – 5 | |||||
| multilevel laminectomy and in situ fusion – 1 | |||||
| Jonsson et al., 1999 | Acta orthopaedica Scandinavica | 8 | Surgery | Cyst excision + | Excellent –5 |
| foraminotomy – 6 | Good – 3 | ||||
| laminectomy – 2 | |||||
| Sabo et al., 1996 | Journal of neurosurgery | 56 | Surgery | Cyst excision + | Excellent – 40 |
| *60 cysts | medial facetectomy – 55 cysts | Poor – 1 | |||
| medial facetectomy + fusion – 6 | *One patient had cyst recurrence and two patients required delayed fusion for post-operative instability | ||||
| Yarde et al., 1995 | Surgical neurology | 8 | Surgery | Cyst excision + | Dramatic pain improvement was seen in seven patients whereas in one patient symptom resolved after redo surgery for removal of scar tissue. |
| hemilaminectomy – 5 | |||||
| laminectomy – 1 | |||||
| laminectomy + fusion –1 | |||||
| fusion – 1 | |||||
| Freidberg et al., 1994 | Neurosurgery | 23 | Surgery | Cyst excision + | Excellent – 15 |
| Considerable improvement – 7 of which 1 required fusion | |||||
| Poor – 1 | |||||
| hemilaminectomy – 13 | |||||
| Laminectomy – 10 | |||||
| Most patients also underwent partial facetectomy |
| Author . | Journal . | No of patients . | Treatment modality . | Procedure . | Outcome . |
|---|---|---|---|---|---|
| Landi et al., 2012 | Neurosurgical review | 15 | Surgery | Cyst excision, hemilaminectomy and medial facetectomy | Complete resolution of symptoms – 12 |
| Improvement in symptoms – 3 | |||||
| Bashir and Ajani, 2012 | World neurosurgery | 21 | Surgery | Cyst excision – 8 | Excellent – 11 |
| Cyst excision + laminectomy – 8 | Good – 5 | ||||
| Cyst excision + laminectomy + fusion – 1 | Fair – 1 | ||||
| *Three patients improved with conservative treatment and 1 patient refused surgery | |||||
| Xu et al., 2010 | Spine | 167 | Surgery | Cyst excision + | Back and radicular pain improved in 91.6% and 91.9% patients |
| facetectomy + instrumented fusion – 56 | |||||
| hemilaminectomy – 51 | *After a mean follow-up of 16 +/– 9 months, 5 patients had recurrent cyst, 36 patients developed recurrent back pain whereas 20 developed recurrent leg pain. | ||||
| bilateral laminectomy – 39 | |||||
| facetectomy + in situ fusion – 18 | |||||
| Boviatsis et al., 2008 | European spine journal | 7 | Surgery | Cyst excision + | Resolution of symptoms – 4 |
| foraminotomy – 3 | Considerable improvement – 3 | ||||
| hemilaminectomy – 2 | |||||
| hemilaminectomy and discectomy – 1 | |||||
| 2 level laminectomy – 1 | |||||
| Weiner et al., 2007 | Journal of orthopaedic surgery and research | 46 | Surgery | Cyst excision + | Resolution of symptoms – 40 |
| *Seven patients later required addition surgery | |||||
| Flavectomy + medial facetectomy + foraminotomy – 23 | |||||
| Flavectomy + medial facetectomy + foraminotomy + fusion – 23 | |||||
| Kusakabe et al., 2006 | Journal of neurosurgery | 45 | Surgery | Cyst excision, flavectomy and medial facetectomy | Resolution of symptoms -45 |
| Metellus et al., 2006 | Acta neurochirurgica | 77 | Surgery | Cyst excision + | Excellent/good – 97.4% |
| partial/total hemilaminectomy proximal foraminotomy and medial facetectomy – 51 | *One patient had cyst recurrence and 1 required fusion for symptomatic spondylolisthesis | ||||
| laminectomy, proximal foraminotomy and medial facetectomy – 26 | |||||
| Khan et al., 2005 | Journal of spinal disorders & techniques | 39 | Surgery | Cyst excision + | Excellent/good – 30 |
| laminectomy + fusion – 26 | Fair/poor – 9 | ||||
| laminectomy – 13 | *Four patients later required fusion procedure whereas 1 patient had cyst recurrence | ||||
| Indar et al., 2004 | Surgeon | 8 | Surgery | Cyst excision, hemilaminotomy, flavectomy and minimal facet joint excision | Excellent – 6 |
| Good – 2 | |||||
| Epstein, 2004 | Spine | 80 | Surgery | Cyst excision + | Excellent/good – 48 |
| Laminectomy + medial facetectomy + foraminotomy – 76 | Fair/poor – 32 | ||||
| Laminectomy + unilateral facetectomy + foraminotomy – 4 | |||||
| *Twelve patients required secondary surgery | |||||
| Pirotte et al., 2003 | Journal of neurosurgery | 46 | Surgery | Cyst excision + | Immediate symptomatic relief was seen in all patients |
| hemilaminectomy – 16 | |||||
| interlaminar decompression – 12 | |||||
| laminectomy – 10 | |||||
| partial hemilaminectomy – 8 | |||||
| Banning et al., 2001 | Spine | 29 | Surgery | Cyst excision and laminotomy was done as primary procedure. | Completely improved – 6 |
| Better – 18 | |||||
| *Two patients later required fusion | |||||
| Two patients also required fusion whereas some others required laminectomy, medial facetectomy and foraminotomy | |||||
| *24/29 response to follow-up | |||||
| Salmon et al., 2001 | Acta neurochirurgica | 28 | Surgery | Cyst excision and medial facetectomy | 26 excellent/good |
| 2 fair/poor | |||||
| Trummer et al., 2001 | Journal of neurology neurosurgery and psychiatry | 19 | Surgery | Cyst excision + | Excellent 17 |
| flavectomy – 8 | Good – 2 | ||||
| hemilaminectomy – 7 | *One patient had cyst recurrence | ||||
| laminectomy – 4 | |||||
| Lyons et al., 2000 | Journal of neurosurgery | 194 | Surgery | Cyst excision –194 + | Good – 134 |
| medial facetectomy – 159 | *47 were lost to follow-up | ||||
| total facetectomy – 23 | *Four patients required delayed fusion for symptomatic spondylolisthesis | ||||
| not specified – 12 | |||||
| + | |||||
| partial hemilaminectomy – 103, | |||||
| total hemilaminectomy/bilateral laminectomy – 86 | |||||
| not specified – 5 | |||||
| 18 patients also had fusion as a primary procedure | |||||
| Howington et al., 1999 | Journal of neurosurgery | 28 | Surgery | Cyst excision + | Resolution of low back pain in 21/26 |
| multilevel laminectomy – 12 | Resolution of leg pain in 19/21 and improved leg pain in 2/21 | ||||
| Partial laminectomy – 10 | |||||
| one-level laminectomy – 5 | |||||
| multilevel laminectomy and in situ fusion – 1 | |||||
| Jonsson et al., 1999 | Acta orthopaedica Scandinavica | 8 | Surgery | Cyst excision + | Excellent –5 |
| foraminotomy – 6 | Good – 3 | ||||
| laminectomy – 2 | |||||
| Sabo et al., 1996 | Journal of neurosurgery | 56 | Surgery | Cyst excision + | Excellent – 40 |
| *60 cysts | medial facetectomy – 55 cysts | Poor – 1 | |||
| medial facetectomy + fusion – 6 | *One patient had cyst recurrence and two patients required delayed fusion for post-operative instability | ||||
| Yarde et al., 1995 | Surgical neurology | 8 | Surgery | Cyst excision + | Dramatic pain improvement was seen in seven patients whereas in one patient symptom resolved after redo surgery for removal of scar tissue. |
| hemilaminectomy – 5 | |||||
| laminectomy – 1 | |||||
| laminectomy + fusion –1 | |||||
| fusion – 1 | |||||
| Freidberg et al., 1994 | Neurosurgery | 23 | Surgery | Cyst excision + | Excellent – 15 |
| Considerable improvement – 7 of which 1 required fusion | |||||
| Poor – 1 | |||||
| hemilaminectomy – 13 | |||||
| Laminectomy – 10 | |||||
| Most patients also underwent partial facetectomy |
The failure rate with conservative treatment is around 47% [6]. Some authors argue that since about 50% of the patients benefit from conservative treatment, a trial of cyst aspiration +/– steroid injection may be considered before opting for more invasive surgical procedure which is associated with higher incidence of post-operative complications. The success rate with surgery is 72–100% [6] but there is no consensus about procedure even if no fusion is being performed. Literature review reveals that authors have tried hemilaminectomy, laminectomy or facetectomy either alone or in combination for treatment of symptomatic LSC. Some others have also attempted minimally invasive resection of LSC with encouraging results (Table 3).
Case series describing minimally invasive surgical management of symptomatic LSC in literature
| Author . | Journal . | No of patients . | Treatment modality . | Procedure . | Outcome . |
|---|---|---|---|---|---|
| Deinsberger et al., 2006 | Journal of spinal disorders and techniques | 31 | Minimally invasive surgery | Cyst excision and flavectomy + | Excellent/good – 80.7% |
| limited bone removal – 27 | |||||
| Standard laminectomy – 4 | |||||
| * Nerve root was decompressed in all patients | |||||
| Sehati et al., 2006 | Neurosurgery focus | 19 | Minimally invasive surgery | Cyst excision + | Excellent – 10 |
| hemilaminectomy – 17 | Good – 8 | ||||
| laminectomy – 2 | Fair – 1 | ||||
| Sandhu et al., 2004 | Neurosurgery | 17 | Minimally invasive surgery | Cyst excision + | Excellent – 14 |
| partial hemilaminectomy + flavectomy – 13 | Good – 2 | ||||
| hemilaminotomy/medial facetectomy – 4 | Poor – 1 |
| Author . | Journal . | No of patients . | Treatment modality . | Procedure . | Outcome . |
|---|---|---|---|---|---|
| Deinsberger et al., 2006 | Journal of spinal disorders and techniques | 31 | Minimally invasive surgery | Cyst excision and flavectomy + | Excellent/good – 80.7% |
| limited bone removal – 27 | |||||
| Standard laminectomy – 4 | |||||
| * Nerve root was decompressed in all patients | |||||
| Sehati et al., 2006 | Neurosurgery focus | 19 | Minimally invasive surgery | Cyst excision + | Excellent – 10 |
| hemilaminectomy – 17 | Good – 8 | ||||
| laminectomy – 2 | Fair – 1 | ||||
| Sandhu et al., 2004 | Neurosurgery | 17 | Minimally invasive surgery | Cyst excision + | Excellent – 14 |
| partial hemilaminectomy + flavectomy – 13 | Good – 2 | ||||
| hemilaminotomy/medial facetectomy – 4 | Poor – 1 |
Case series describing minimally invasive surgical management of symptomatic LSC in literature
| Author . | Journal . | No of patients . | Treatment modality . | Procedure . | Outcome . |
|---|---|---|---|---|---|
| Deinsberger et al., 2006 | Journal of spinal disorders and techniques | 31 | Minimally invasive surgery | Cyst excision and flavectomy + | Excellent/good – 80.7% |
| limited bone removal – 27 | |||||
| Standard laminectomy – 4 | |||||
| * Nerve root was decompressed in all patients | |||||
| Sehati et al., 2006 | Neurosurgery focus | 19 | Minimally invasive surgery | Cyst excision + | Excellent – 10 |
| hemilaminectomy – 17 | Good – 8 | ||||
| laminectomy – 2 | Fair – 1 | ||||
| Sandhu et al., 2004 | Neurosurgery | 17 | Minimally invasive surgery | Cyst excision + | Excellent – 14 |
| partial hemilaminectomy + flavectomy – 13 | Good – 2 | ||||
| hemilaminotomy/medial facetectomy – 4 | Poor – 1 |
| Author . | Journal . | No of patients . | Treatment modality . | Procedure . | Outcome . |
|---|---|---|---|---|---|
| Deinsberger et al., 2006 | Journal of spinal disorders and techniques | 31 | Minimally invasive surgery | Cyst excision and flavectomy + | Excellent/good – 80.7% |
| limited bone removal – 27 | |||||
| Standard laminectomy – 4 | |||||
| * Nerve root was decompressed in all patients | |||||
| Sehati et al., 2006 | Neurosurgery focus | 19 | Minimally invasive surgery | Cyst excision + | Excellent – 10 |
| hemilaminectomy – 17 | Good – 8 | ||||
| laminectomy – 2 | Fair – 1 | ||||
| Sandhu et al., 2004 | Neurosurgery | 17 | Minimally invasive surgery | Cyst excision + | Excellent – 14 |
| partial hemilaminectomy + flavectomy – 13 | Good – 2 | ||||
| hemilaminotomy/medial facetectomy – 4 | Poor – 1 |
Spontaneous regression of symptomatic LSC is uncommon and has only been reported on a handful of occasions (Table 4). Factors which may contribute to spontaneous disappearance are extrusion of contents of the cyst and resorption of cyst wall or changes in local forces which initially led to synovial cyst formation [9, 10]. Synovial cysts show a female preponderance, so it is not surprising that most cases of spontaneous regression of symptomatic LSC have been reported in female patients. Our case of spontaneous regression of symptomatic LSC adds to the growing list of such cases and may help in understanding the natural history of the disease process in future. Also as there is controversy regarding optimal management of symptomatic LSC and few reports of spontaneous regression, there may be an argument for managing some patients conservatively with wait and watch approach.
| Author . | Journal . | Year . | Patient's age/sex . | Spinal level . |
|---|---|---|---|---|
| Mercader et al. | Neuroradiology | 1985 | 65 years/female | L4/L5 |
| Maezawa et al. | European spine journal | 2000 | 15 years/male | L4/L5 |
| Swartz et al. | American journal of neuroradiology | 2003 | 58 years/female | L5/S1 |
| Houten et al. | Journal of neurosurgery | 2003 | 64 years/male | L4/L5 |
| 57 years/female | L4/L5 | |||
| 58 years/female | L4/L5 | |||
| Ewald et al. | Zentralblatt fur neurochirurgie | 2005 | 65 years/female | L4/L5 |
| Illerhaus et al. | RoFo: Fortschritte auf dem gebiete der rontgenstrahlen und der nuklearmedizin | 2005 | 50 years/female | L4/5 |
| Pulhorn and Murphy | British journal of neurosurgery | 2012 | 72 years/female | L4/5 |
| Author . | Journal . | Year . | Patient's age/sex . | Spinal level . |
|---|---|---|---|---|
| Mercader et al. | Neuroradiology | 1985 | 65 years/female | L4/L5 |
| Maezawa et al. | European spine journal | 2000 | 15 years/male | L4/L5 |
| Swartz et al. | American journal of neuroradiology | 2003 | 58 years/female | L5/S1 |
| Houten et al. | Journal of neurosurgery | 2003 | 64 years/male | L4/L5 |
| 57 years/female | L4/L5 | |||
| 58 years/female | L4/L5 | |||
| Ewald et al. | Zentralblatt fur neurochirurgie | 2005 | 65 years/female | L4/L5 |
| Illerhaus et al. | RoFo: Fortschritte auf dem gebiete der rontgenstrahlen und der nuklearmedizin | 2005 | 50 years/female | L4/5 |
| Pulhorn and Murphy | British journal of neurosurgery | 2012 | 72 years/female | L4/5 |
| Author . | Journal . | Year . | Patient's age/sex . | Spinal level . |
|---|---|---|---|---|
| Mercader et al. | Neuroradiology | 1985 | 65 years/female | L4/L5 |
| Maezawa et al. | European spine journal | 2000 | 15 years/male | L4/L5 |
| Swartz et al. | American journal of neuroradiology | 2003 | 58 years/female | L5/S1 |
| Houten et al. | Journal of neurosurgery | 2003 | 64 years/male | L4/L5 |
| 57 years/female | L4/L5 | |||
| 58 years/female | L4/L5 | |||
| Ewald et al. | Zentralblatt fur neurochirurgie | 2005 | 65 years/female | L4/L5 |
| Illerhaus et al. | RoFo: Fortschritte auf dem gebiete der rontgenstrahlen und der nuklearmedizin | 2005 | 50 years/female | L4/5 |
| Pulhorn and Murphy | British journal of neurosurgery | 2012 | 72 years/female | L4/5 |
| Author . | Journal . | Year . | Patient's age/sex . | Spinal level . |
|---|---|---|---|---|
| Mercader et al. | Neuroradiology | 1985 | 65 years/female | L4/L5 |
| Maezawa et al. | European spine journal | 2000 | 15 years/male | L4/L5 |
| Swartz et al. | American journal of neuroradiology | 2003 | 58 years/female | L5/S1 |
| Houten et al. | Journal of neurosurgery | 2003 | 64 years/male | L4/L5 |
| 57 years/female | L4/L5 | |||
| 58 years/female | L4/L5 | |||
| Ewald et al. | Zentralblatt fur neurochirurgie | 2005 | 65 years/female | L4/L5 |
| Illerhaus et al. | RoFo: Fortschritte auf dem gebiete der rontgenstrahlen und der nuklearmedizin | 2005 | 50 years/female | L4/5 |
| Pulhorn and Murphy | British journal of neurosurgery | 2012 | 72 years/female | L4/5 |
Management of symptomatic LSC should be on a case to case basis depending upon presenting signs and symptoms, radiological findings, surgeon's expertise and patient's aspirations. Most studies show that surgery is superior to conservative management, however, as far as answer to the important question of ‘to fuse or not to fuse’ – the jury is still out. A randomized control trial may be needed to decide the optimal treatment for symptomatic LSC.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES



