-
PDF
- Split View
-
Views
-
Cite
Cite
M.L. Gueye, O. Thiam, M. Seck, M.N. Gueye, A.O. Toure, M. Cisse, O. Ka, M. Dieng, C.T. Toure, Perforated mesenteric Meckel's diverticulum in an adult: a real variant?, Journal of Surgical Case Reports, Volume 2015, Issue 9, September 2015, rjv115, https://doi.org/10.1093/jscr/rjv115
Close - Share Icon Share
Abstract
A Meckel's diverticulum is the most common congenital anomaly of the gastrointestinal tract. It is a real diverticulum that is usually located on the anti-mesenteric edge in the last meter of the ileum. Its location on the mesenteric edge has been rarely reported. It may lead to several complications including perforation that may be life-threatening for the patient. We report herein a case of perforated mesenteric Meckel's diverticulum in an adult patient. Upon surgical exploration by laparotomy, we found a perforated Meckel's diverticulum located on the mesenteric edge of the ileum 60 cm from the ileocoecal junction and 400 ml of seropurulent peritoneal fluid. The patient underwent a segmental ileal resection and an end-to-end anastomosis. The postoperative outcomes were marked by a persistent peritonitis that required successful revision surgery.
INTRODUCTION
Meckel's diverticulum is an embryonic residue of the omphalomesenteric duct [1]. It is by far the most common congenital malformation of the gastrointestinal tract [1]. It is a real ileal diverticulum usually located on the anti-mesenteric edge in the last meter of the small bowel [2]. It may lead to several complications including perforation. The location on the ileal mesenteric edge has been rarely reported and remains controversial [1, 2]. Indeed, it raises the question about the differential diagnosis with bowel duplication which is still not elucidated. We report a case of perforated Meckel's diverticulum that was located on the mesenteric edge of the ileum. We discuss the embryological aspects and the therapeutic modalities of this entity.
CASE REPORT
A 45-year-old patient admitted to the emergency unit was complaining of abdominal pain lasting for 3 days. Initially, the pain was located in the epigastric region, then secondarily generalized to the whole abdomen. He also reported vomiting related to food intake and bowel habit change. Physical examination revealed a good general condition, a temperature of 38.8 C°, a pulse rate of 120 heart beats/min, a blood pressure of 100/90 mmHg and a respiratory frequency of 28 cycles/min. There was an abdominal distension with a widespread tenderness. Plain abdominal radiography showed air-fluid levels and was suggestive of abdominal effusion (Fig. 1). On biology, blood cell count was 12 400 cells/mm3 (normal range: 4000–10 000) and creatinine was 16.8 mg/l (normal range: 6–12). A generalized peritonitis was then suspected, and a laparotomy was performed. On exploration, we found 400 ml of seropurulent peritoneal fluid and a perforated Meckel's diverticulum of 3.5 cm in size, which was located 60 cm from the ileocecal junction on the mesenteric edge of the ileum (Fig. 2). The patient underwent a removal of the diverticulum by a segmental resection of the ileum with an end-to-end anastomosis. The postoperative course was marked by persistent peritonitis, which motivated a revision surgery that involved a peritoneal lavage and drainage. Second, the postoperative course was uneventful. Pathological examination of the surgical specimen found a perforated diverticulitis without heterotopic tissue.

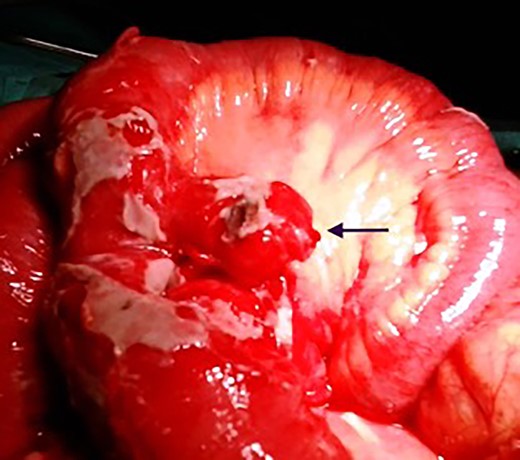
Intraoperative findings of perforated mesenteric Meckel diverticulum.
DISCUSSION
The Meckel's diverticulum is the most common birth defect of the gastrointestinal tract [1]. It results from the incomplete regression of the omphalomesenteric duct that connects the primitive intestine to the yolk sac during the embryonic period [1, 3]. It is usually asymptomatic and may lead to complications such as perforation [3]. The location of this diverticulum on the anti-mesenteric ileal edge has been for a long recognized as diagnostic criterion [1, 2, 4]. However, some cases of location on the mesenteric ileal edge have been reported since 1941 and so were suggestive of possible ileal duplication [1, 2, 4]. Meckel's diverticulum with mesenteric location can be subserosal or intra-mesenteric [5]. In our patient, it was a subserous diverticulum. While in intra-mesenteric variety, transillumination of the mesentery is necessary to highlight the diverticulum [5]. The persistence of a short vitelline artery is thought to be implicated in the pathophysiology of mesenteric diverticula [2, 5]. Indeed, this artery yolk could in part explain the diverticular meso, which, in case of rapid growth, causes a pull on the diverticulum and then a migration of its base to the mesenteric edge [2, 5]. The main differential diagnosis in these cases is the ileal duplication where vascularization is dependent on the ileal vascularization, while the mesenteric diverticulum's vascularization is most often provided by a vitelline artery [1, 2]. However, most authors do not consider vascularization as a differential diagnosis tool because the vitelline artery presents in only 10% of cases [1, 2]. This hypothesis is supported by Kurzbart et al., who reported a case of omphalomesenteric duct persistence detected in the neonatal period that fell to the age of 3 months and became a Meckel's diverticulum without mesenteric diverticular meso [6].
In our patient, as well as in Buke's one, pathological examination of the surgical specimen did not show meso or diverticular sac artery. Carpenter et al., meanwhile, found a vitelline artery on CT scan [1]. According to Buke et al., a complete regression of the vitelline artery or a clot in utero between the mesentery and the omphalomesenteric duct might also explain this anatomical variant [2]. Perforation of Meckel's diverticulum is a main cause of right lower quadrant pain as well as appendicitis. If the systematic resection of incidental Meckel diverticula is not unanimous, resection of complicated diverticula is widely agreed [3]. According to Park et al., a diverticulectomy can be achieved if there is no mass suggestive of heterotopic tissue [3]. However, given that the risk of degeneration of these tissues that may go unnoticed, segmental ileal resection seems to be the best option to adopt. It may be followed by an ileal anastomosis when local conditions allow it. In our patient, it was realized a segmental ileal resection followed by an end-to-end anastomosis. The postoperative course was marked by a persistent peritonitis probably due to a peritoneal toilet failure. In case of massive contamination of the peritoneal cavity, an ileostomy associated with an abundant peritoneal lavage is the most prudent option.
Mesenteric Meckel's diverticulum is a rare variant of Meckel's diverticulum. Its distinction with ileal duplication is still controversial. Segmental ileal resection seems to be the ideal therapeutic attitude given the possible presence of heterotopic tissues. In case of perforation, resection and ileostomy should be performed especially if the peritoneal cavity is septic.
CONFLICT OF INTEREST STATEMENT
None declared.



