-
PDF
- Split View
-
Views
-
Cite
Cite
Diana H. Liang, Wade R. Rosenberg, Sylvia Martinez, Bypass grafting between the supraceliac aorta and the common hepatic artery during pancreaticoduodenectomy, Journal of Surgical Case Reports, Volume 2015, Issue 9, September 2015, rjv107, https://doi.org/10.1093/jscr/rjv107
Close - Share Icon Share
Abstract
Patients with celiac artery stenosis often remain asymptomatic due to formation of extensive collateral pathways. Hepatic or anastomotic ischemia may occur when the gastroduodenal artery and these collaterals are ligated during pancreaticoduodenectomy. Here, we present a patient with severe atherosclerotic disease of the celiac axis who successfully underwent pancreaticoduodenectomy with aorto-hepatic bypass.
INTRODUCTION
Celiac artery stenosis is a relatively common condition with an incidence estimated to be between 10 and 25% of the adult population. However, many patients remain asymptomatic until the arterial blood flow is reduced by 60–70%, due to the development of extensive collateral pathways [1]. During pancreaticoduodenectomy, the gastroduodenal artery and its collaterals are ligated, and if not managed properly, catastrophic complications, such as hepatic and/or anastomotic ischemia, may result [2]. In this study, we present an elderly patient with pancreatic adenocarcinoma and severe atherosclerosis who successfully underwent pancreaticoduodenectomy with bypass grafting between the supraceliac aorta and the common hepatic artery.
CASE REPORT
An 83-year-old male patient presented with a chief complaint of painless jaundice. His medical history was significant for lung cancer, bladder cancer, coronary artery disease and history of femoral popliteal bypass surgery for severe peripheral vascular disease. On initial presentation, the patient was afebrile, normotensive and in sinus rhythm. He exhibited no tenderness on abdominal examination. The biochemical studies were significant for a total bilirubin of 5.3 mg/dl, a direct bilirubin of 4.5 mg/dl and an alkaline phosphatase of 561 U/l. Abdominal ultrasound showed a 17-mm common bile duct (CBD) dilatation and moderate intrahepatic ductal dilatation. Magnetic resonance imaging showed a high-grade stricture of the distal CBD, resulting in markedly dilated intrahepatic bile ducts, with 2.6 cm by 1.9 cm soft-tissue fullness at the level of the pancreatic head (Fig. 1A). Abdominal angiography showed moderate narrowing at the origin of the celiac artery; however, the distal celiac, superior mesenteric and inferior mesenteric arteries were patent (Fig. 1B). Positron emission tomography–computed tomography showed no recurrent disease of lung and bladder cancer and no significantly abnormal uptake within the pancreatic lesion. Endoscopic retrograde cholangiopancreatography was performed with sphincterotomy, CBD dilatation and concurrent placement of a 7-cm, 10-Fr stent.
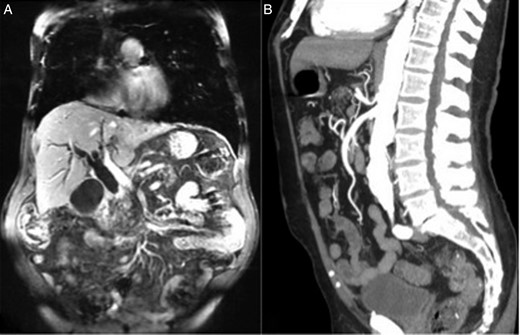
(A) MRI of the abdomen demonstrated marked intrahepatic biliary dilatation due to an abrupt high-grade stricture of the distal CBD at the level of the pancreatic head. (B) CT angiography of the abdomen showed patent celiac artery despite moderate narrowing at the origin of the celiac artery.
With no evidence for systemic disease, pancreaticoduodenectomy was recommended. The mobilization, dissection and division of the jejunum, stomach and pancreas were performed in the standard fashion. Manual compression of the gastroduodenal artery did not show any evidence of loss of blood flow to the common hepatic artery. After the neck of the pancreas was divided, the tumor appeared to be adherent to the right lateral wall of the portal vein. Thus, the portal vein was dissected above and below the area of the tumor, and the sidewall of the portal vein was excised and repaired. After the completion of pancreaticojejunostomy, the hepatic artery was found to be soft and nonpulsatile, with significantly diminished blood flow on Doppler ultrasound. However, there was no evidence of arterial injury and no evidence of gross visceral ischemia. At this time, the hepaticojejunostomy and the gastrojejunostomy were performed in the usual fashion. After completion of the anastomoses, the hepatic artery continued to be nonpulsatile. Therefore, a bypass from the supraceliac aorta to the common hepatic artery was created to prevent potential postoperative complications, including anastomotic ischemia and breakdown. The supraceliac aorta was dissected. After the patient was given intravenous heparin, a 6-mm GORE-TEX graft was anastomosed to the aorta and to the hepatic artery in an end-to-side fashion. Intraoperative Doppler confirmed reliable pulsatile flow in the hepatic artery distal to the anastomosis.
Surgical pathology showed stage IIB poorly differentiated pancreatic adenocarcinoma with extensive perineural invasion, focal lymphovascular invasion and metastatic carcinoma in 1 of 30 lymph nodes. The patient had an uneventful postoperative course and was discharged 7 days after the operation. Postoperatively, patient underwent adjuvant chemotherapy and radiation.
DISCUSSION
Up to 5% of patients undergoing pancreaticoduodenectomy are estimated to have celiac artery stenosis. In these patients, extensive collaterals develop from the superior mesenteric artery to provide retrograde flow from the gastroduodenal artery to the liver [3]. Although the vast majority of these patients are asymptomatic, the collaterals and gastroduodenal artery are transected during pancreaticoduodenectomy and may cause hepatic and/or anastomotic ischemia, unless intervention is undertaken in a timely fashion [2, 3].
Classically, the gastroduodenal artery occlusion test has been performed to assess for adequate blood flow, as this artery represents the communication between the celiac axis and the superior mesenteric artery. If visceral ischemia becomes evident upon occlusion of the gastroduodenal artery, a revascularization procedure is necessary. Unfortunately, there are times when this test is negative and visceral ischemia is seen only after the pancreatic resection, due to the interruption of collateral flow from pancreaticoduodenal blood supply. Machado et al. [4] proposed an additional maneuver of occluding pancreatic flow at the pancreatic neck after the portal vein dissection. This maneuver interrupts collateral vessels between the pancreatic body and the splenic arterial system and may increase the sensitivity of the gastroduodenal artery occlusion test.
The first case of successful pancreaticoduodencetomy in the setting of celiac occlusive disease was reported in 1980, using a splenic-to-superior mesenteric artery reimplantation technique [5]. These authors also noted that the gastroduodenal artery occlusion test is not always a reliable test and recommended preoperative arteriographic evaluation.
Since pancreaticoduodenectomy is the only potentially curative option for pancreatic cancer, patients with significant mesenteric arterial disease and pancreatic cancer should be offered a combined pancreaticoduodenectomy and revascularization procedure. There are several revascularization options reported in the literature. Others have reported creation of an anastomosis between the superior posterior pancreaticoduodenal artery and the posterior inferior pancreaticoduodenal artery, anastomosis between the middle colic artery and the gastroduodenal artery, and transposition of the celiac artery onto the superior mesenteric artery [6–8]. In our case, bypass grafting between the supraceliac aorta and the hepatic artery proved to be a successful option for our patient.
FUNDING
This research was supported by the Department of Surgery at Houston Methodist Hospital.



