-
PDF
- Split View
-
Views
-
Cite
Cite
Sugong Chen, Sanda A. Tan, Wonwoo Shon, Christiana M. Shaw, Cylindroma-like basaloid anal cancer presenting as a large pelvic mass in a patient with ulcerative colitis, Journal of Surgical Case Reports, Volume 2015, Issue 7, July 2015, rjv093, https://doi.org/10.1093/jscr/rjv093
Close - Share Icon Share
Abstract
Basaloid cancers of the lower gastrointestinal tract are rare. The lack of mucosal involvement of this type of tumor is uncharacteristic and, to our knowledge, has not been described. In addition, the cylindroma-like appearance of this cancer has only a few examples in the literature. A 51-year-old male presented to us with a history of ulcerative colitis (UC) and obstruction of the anal canal. Imaging and colonoscopy revealed an entirely extraluminal tumor. Percutaneous biopsy yielded a diagnosis of cylindroma-like basaloid carcinoma of the anal region. Neoadjuvant chemotherapy and radiation resulted in stable disease by RECIST criteria. Surgical planning ensued, which led to R0 resection of the tumor, total colectomy and end ileostomy for his UC, and reconstruction of the perineal defect with a rectus myocutaneous flap. Surveillance at 6 months demonstrated no evidence of disease.
INTRODUCTION
Anal basaloid carcinoma is an uncommon malignancy in the lower alimentary tract. We present an atypical presentation of this disease with rare pathological finding in the setting of ulcerative colitis (UC). This patient came to our institution as a referral for management of worsening colitis and difficulty passing stool. Initial colonoscopic and radiographic studies revealed a large mass in the right ischiorectal fossa that appeared entirely extraluminal without pathological evidence of mucosal dysplasia. Concern was raised for a soft tissue sarcoma until percutaneous biopsy of the mass demonstrated a cylindroma-like basaloid carcinoma of the anal region.
CASE REPORT
A 51-year-old Caucasian male with 20-year history of UC presents with decreased stool caliber, inability to empty completely, as well as bloody stools. His UC was well controlled until the previous year, at which point he required the addition of oral mesalamine and hydrocortisone suppositories. Recent colonoscopy visualized left-sided disease, and biopsies did not reveal any dysplasia. Magnetic resonance imaging (MRI) and computed tomography (CT) showed a large soft tissue mass in the right ischiorectal fossa with mass effect on the pelvic diaphragm muscles, prostate and rectum (Fig. 1). It had the appearance of a soft tissue sarcoma. However, CT-guided percutaneous biopsy of the mass revealed a cylindroma-like basaloid carcinoma of the anal region. It was at Stage II, T3N0M0, according to American Joint Committee on Cancer guidelines. He received 5 weeks of radiation (54 Gy), plus chemotherapy with 5-fluorouracil (5FU) and mitomycin C during Weeks 1 and 5 of radiation with only a modest response (20%). Extirpation was planned. Given his history of UC, we performed total colectomy and end ileostomy in conjunction with wide abdominoperineal resection of the tumor. Genitourinary structures and the bony pelvis were spared. We reconstructed his perineum with a rectus abdominis myocutaneous flap from the left abdomen, and the omentum was used to obliterate pelvic space. The ileostomy was placed on the right abdomen (Fig. 2).
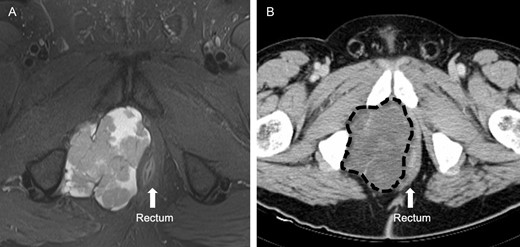
(A) This is a MRI T2-weighted image before neoadjuvant therapy. The light area clearly delineates the large heterogeneous mass in the right ischiorectal fossa. The rectum is displaced to the left. (B) This is a CT image of the same mass after neoadjuvant therapy, marked by dashed line.
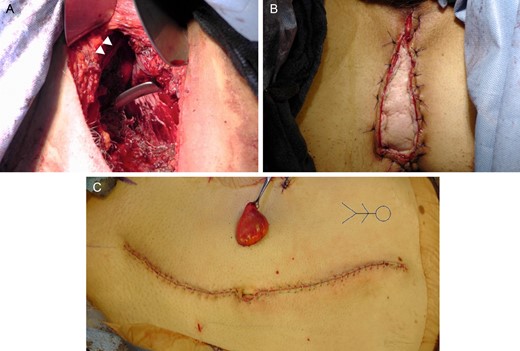
(A) Perineum wound after removal of specimen. White arrowheads mark the inferior pubic ramus. (B) Rectus abdominis myocutaneous flap reconstruction of the perineum. (C) Abdominal closure with end ileostomy. Rectus flap was harvested from the left side. Stick figure marks patient orientation.
Pathology demonstrated complete R0 oncologic resection. Microscopically, the tumor showed a proliferation of basaloid cells arranged in a trabecular and nested growth pattern. The neoplastic cells had hyperchromatic nuclei with minimal cytoplasm and mild pleomorphism (Fig. 3A). There were scattered mitotic figures and areas of tumoral necrosis. There was no evidence of dysplasia in the overlying rectal and anal epithelia. In some areas, the lesion also exhibited a jigsaw puzzle (mosaic-like) arrangement of basaloid cells surrounded by bright eosinophilic hyaline basement membrane material, simulating cylindroma of the skin or adenoid cystic carcinoma. By immunohistochemistry, the lesional cells were positive for CK7 and partially positive for p16 (Fig. 3B). Areas of patchy high-molecular-weight keratin immunoreactivity were also observed. CK20, monoclonal CEA, CD117, calponin, S-100 and p40 stains were completely negative. Finally, all 15 regional lymph nodes were negative for metastatic carcinoma.
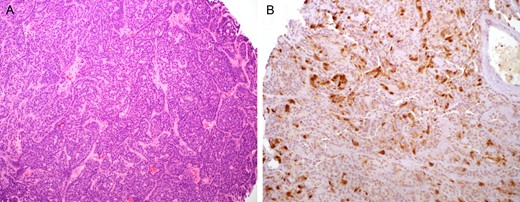
Basaloid carcinoma of the anal canal. (A) Relatively small basaloid neoplastic cells arranging in a trabecular pattern, resembling cylindroma of the skin or adenoid cystic carcinoma. (B) Scattered tumor cells with p16 immunoreactivity.
No adjuvant therapy was planned. He was recently seen at his 6-month postoperative follow-up with no evidence of recurrent disease on imaging, although he reported loss of sexual function and mild urinary incontinence.
DISCUSSION
Anal cancer accounts for 2.4% of malignancies of the digestive tract. This includes cancers of the anorectal canal and anal margin. In 2014, the American Cancer Society estimates 7210 new cases of anal cancer and 950 deaths [1]. Nearly half of all anal cancers are squamous cell carcinomas. About a third are basaloid carcinomas (otherwise known as cloacogenic or transition cell tumors) [2]. Adenocarcinoma, mucinous adenocarcinoma, melanoma and others are rare [2]. Human papilloma virus (HPV) infection is postulated to be a prerequisite for anal cancer development, and markers for HPV infection are found in the vast majority of tumor specimens [3, 4].
In the rectum and anal canal, only a few examples of basaloid carcinomas with cylindromatous microcystic spaces or spiradenocylindroma-like pattern have been reported [5–7]. The clinical significance and associated pathologic variables of this unusual morphologic pattern in basaloid anal carcinomas are uncertain at this point. Notably, Kacerovska and colleagues previously detected the presence of HPV-16 in the lesional tissue, thus indicating HPV as a potential causative factor [7]. In our case, the tumor cells were also partially highlighted by p16 immunohistochemistry, a surrogate marker for transcriptionally active HPV. However, strong and diffuse p16 expression can be observed in the absence of HPV E6/E7 mRNA expression [8]. Therefore, additional molecular confirmation will be necessary in establishing the presence of high-risk HPV in our case.
This patient's tumor was entirely extraluminal, which allowed it to grow to a large size before detection. Obstruction from external compression was his main complaint. Lower gastrointestinal bleeding, although present at the time of diagnosis, was likely a result of his colitis and unrelated to his tumor. In terms of risk factors, aside from his HPV positivity, inflammatory bowel disease (IBD) is also known to be associated with tumorigenesis. The chronic inflammatory state and long-term use of immunosuppressive therapy are thought to be causative factors. Although there is no clear evidence to suggest that incidence of anal cancer is higher in the IBD population, an association is likely [9]. In this patient, colectomy was indicated because UC significantly increases his risk for developing colon cancer, and chemoradiation may exacerbate symptoms of colitis.
Fortunately, his cancer was discovered at an early stage, and because of the case complexity, surgical resection was planned in advance involving surgical oncology, colorectal surgery, urology, orthopedic surgery, and plastic and reconstructive surgery. Although he had a modest response to neoadjuvant therapy, a R0 resection was accomplished while preserving his genitourinary and skeletal anatomy. Flap reconstruction was planned in advance in anticipation of poor primary tissue healing as a result of radiation and the large defect in his perineum after extirpation. Likewise, the colectomy and ileostomy portions of the operation were planned to ensure the integrity of the rectus flap. Postoperatively, he had mild perineal pain that had resolved at 3 months postoperatively and sustained some functional deficit of the genitourinary system. The multidisciplinary approach was continued in his postoperative care and surveillance.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- malignant neoplasm of anus
- biopsy
- cancer
- carcinoma
- colonoscopy
- ulcerative colitis
- adenoid cystic carcinoma
- anogenital region
- reconstructive surgical procedures
- surgical procedures, operative
- diagnosis
- diagnostic imaging
- mucous membrane
- neoplasms
- pelvic mass
- gastrointestinal tract
- anal carcinoma
- anal canal
- myocutaneous flap
- surveillance, medical
- colectomy, total
- stoma, end ileostomy
- perianal region
- chemotherapy, neoadjuvant
- response evaluation criteria in solid tumors



