-
PDF
- Split View
-
Views
-
Cite
Cite
Ruelan V. Furtado, Trevor J. D'Netto, Henry C. Hook, Gregory L. Falk, SarahJayne Vivian, Massive hiatus hernia complicated by jaundice, Journal of Surgical Case Reports, Volume 2015, Issue 7, July 2015, rjv087, https://doi.org/10.1093/jscr/rjv087
Close - Share Icon Share
Abstract
Giant para-oesophageal hernia may include pancreas with pancreatic complication and rarely jaundice. Repair is feasible and durable by laparoscopy. Magnetic resonance cholangiopancreatography is diagnostic.
INTRODUCTION
Herein reported a patient presenting with jaundice ultimately proving caused by a giant hiatus hernia also containing pancreas, and repaired successfully by laparoscopy.
CASE REPORT
A 59-year-old farmer presented with pain and obstructive jaundice. There were two recent episodes of post-prandial chest pain and vomiting with regurgitation of retained food. There was a history of early satiety, non-progressive dysphagia and significant weight loss in preceding months. There was no chest pain suggesting gastric volvulus.
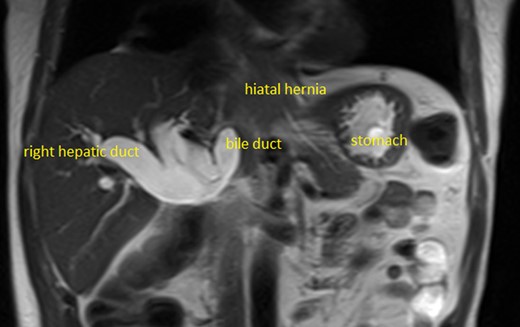
The bilirubin was 158 µmol per litre and the alkaline phosphatase 751 IU/l, gamma glutamyl transferase (GGT) 1560 IU/l, aspartate aminotransferase 110 IU/l, and there was a normocytic anaemia (haemoglobin 130 3G/L). Computed tomography (CT) scan showed a massive hiatus hernia (MHH) containing duodenum and pancreas, and intra- and extra-hepatic biliary dilatation. The bile duct was not obtained at endoscopic retrograde cholangiopancreatography (ERCP), and the ampulla was normal. Magnetic resonance cholangiopancreatography (MRCP) showed a dilated biliary tree with axis deviation of the common bile duct (CBD) causing obstruction and kinking and proximal dilatation, where it entered the hiatal opening (Fig. 1).
At laparoscopy, the pancreas was seen entering the hiatus hernia (Fig. 2). Dissection of the sack allowed reduction in all hernia contents. The oesophagus was mobilised into the mediastinum, and the cardia was drawn without tension into the abdomen. Posterior and anterior repair of the hiatus was performed with 0 Ethibond. Total fundoplication and cardiopexy were performed as described by D'Netto et al. [1]. The patient left hospital 48 h after the procedure taking a full fluid diet. The bilirubin progressively returned to normal over 3 weeks. At 3-year follow-up, there were no symptoms and barium meal showed no recurrence.
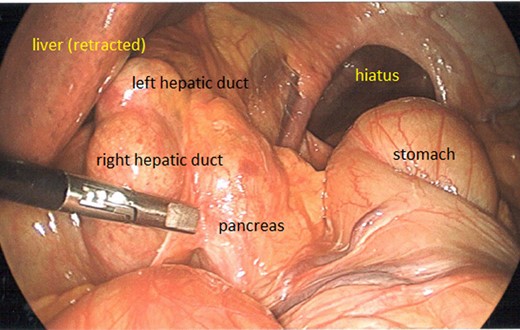
Intraoperative: pancreas seen herniated through hiatus. CBD dilated.
DISCUSSION
Hiatus hernia is graded in four types. Type 1 sliding, Type 2 pure para-oesophageal, Type 3 mixed para-oesophageal and Type 4 mixed para-oesophageal with another organ also herniated in the chest (usually colon). Affected patients frequently may present with symptoms of early satiety, dysphagia, atypical chest pain, dyspnoea and iron deficiency anaemia [2]. Incarceration of the pancreas is rare; however, pancreatitis has been reported as a presenting symptom due to obstruction of the duct of Wirsung [3].
This case illustrates an unusual cause of jaundice and the feasibility of repair by laparoscopy even when the pancreas is present in the chest [4]. Diagnosis was greatly facilitated by magnetic resonance imaging (MRI)/MRCP, and ERCP was technically difficult due to the position of the duodenum. The relationship between the hiatus, hernia and bile duct was well visualised confirming clinical suspicion. Occasional reports are present in the literature of pancreatic herniation causing jaundice in MHH [5–7].
CONFLICT OF INTEREST STATEMENT
None declared.



