-
PDF
- Split View
-
Views
-
Cite
Cite
Animesh A. Singla, Danielle McPherson, Apresh A Singla, Jane Cross, Anthony Leslie, External iliac artery occlusion in a paediatric patient following handlebar trauma, Journal of Surgical Case Reports, Volume 2015, Issue 3, March 2015, rjv015, https://doi.org/10.1093/jscr/rjv015
Close - Share Icon Share
Abstract
Arterial occlusion following blunt trauma is an uncommon occurrence. We report an unusual case of delayed external iliac artery occlusion in a young male following blunt abdominal injury. He was successfully treated with thromboendarterectomy and saphenous vein patch repair. There have only been a handful of documented cases occurring in the paediatric population. All patients presenting with groin injury from this mechanism should be carefully investigated and monitored for risk of vascular injury.
INTRODUCTION
Traumatic arterial occlusion following major or minor blunt trauma, especially in the absence of any other bony injury, is a rare phenomenon [1]. ‘Motor-scooter handlebar syndrome’ is one such type of arterial occlusion affecting vascular structures following direct blow by a handlebar of a motorbike or bicycle to the groin. Given their superficial course at this location, femoral vessels are the most common vascular structures affected. In all instances, injury to iliac vessels remains exceedingly rare, given its posterior position within the pelvis, representing only 0.4% of vascular injuries [2].
In this case, we highlight a delayed presentation of external iliac artery occlusion secondary to ‘motor-scooter handlebar syndrome’, in a paediatric patient. Pathophysiology and management of vascular injuries in the paediatric population vary significantly compared with the adult population. Additional factors which need to be considered include: smaller vessel size or vessel spasm, higher risk of infection, tendency for re-stenosis and continuing growth. We review previous paediatric cases of this unusual vascular injury to highlight the pathology and most appropriate management option.
CASE REPORT
A 15-year-old male presented to the emergency department following a direct blow from his bicycle handlebars to his groin. His chief complaint was pain and swelling in the right inguinal region. His abdominal examination was unremarkable, except for a small abrasion and visible mass in his right groin. Peripheral pulses were palpable bilaterally. After exclusion of other abdominal or chest injuries, he was discharged on the same day with a diagnosis of right groin haematoma and follow-up in 6–8 weeks.
He presented to his general practitioner 2 weeks later with claudication. His symptoms included pain and paraesthesia in his right buttocks on mobilization >100 m. He was found to have absent peripheral pulses in his right leg, although it appeared well perfused with a normal capillary refill. An arterial Doppler ultrasound showed a right external iliac artery thrombus occluding the proximal two-thirds of the vessel. A computed tomography scan of the abdomen and pelvis with intravenous contrast identified complete occlusion of the right external iliac artery ∼1 cm beyond its origin. However, the common femoral artery and profunda femoris remained patent via collaterals (Fig. 1).

He underwent a right external iliac thromboendarterectomy with patch repair using a saphenous vein graft. A suprainguinal incision was initially made in attempt to expose the proximal external iliac artery. Due to its extent, retrieval of the entire thrombus was incomplete and a second groin incision near the junction of the common femoral with external iliac (at the inguinal ligament level) was required. The patient subsequently underwent a proximal and distal thrombectomy, and the arteriotomy was extended between the two incisions identifying an intimal stricture with significant fibrosis (Fig. 2). An intimal flap was identified in the distal region and tacked down with a 7-0 prolene suture. The long saphenous vein was harvested and the defect closed with patch repair extending from proximal iliac to proximal femoral vessel. He had an uneventful recovery. At the initial 2-week follow-up, the vessels remained patent and patient was progressing well. Subsequently, regular biannual follow-up was planned to monitor for any longer-term complications.
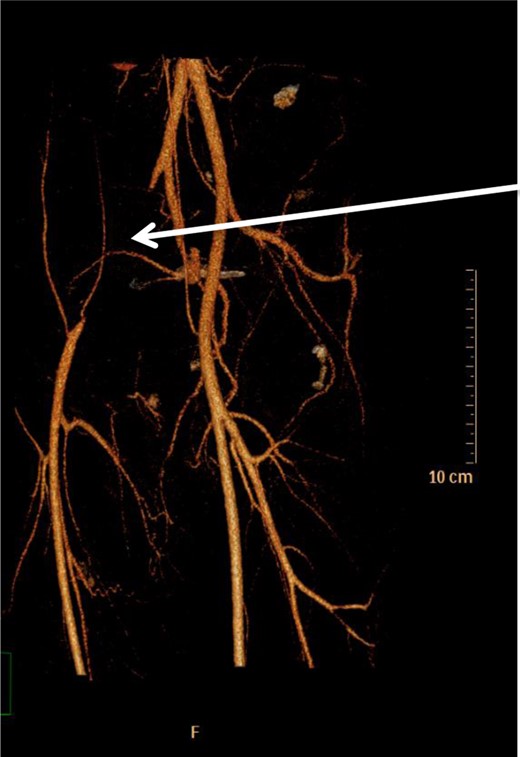
Occlusion of right external iliac artery 1 cm below its origin (white arrow). The right common femoral artery is supplied by inferior epigastric and lateral thigh collaterals. Left-sided vessels are normal.
DISCUSSION
‘Motor-scooter handlebar syndrome’ is an uncommon form of arterial blunt injury following a direct blow by the handlebar of motorbikes or bicycles [3]. Only a handful of paediatric cases have been reported [1, 2, 4–7]. The common femoral vessel is the most commonly affected vascular structure. A common site for these injuries is at the inguinal ligament, where the femoral artery is superficial and courses anterior to the superior pubic ramus and femoral head. As such, it is prone to compression between the handlebar and posterior osseous structures. In addition, it is a relatively immobile structure, tethered by arterial branches, periadventitial connective tissue and the femoral sheath [8].
Several pathological mechanisms have been identified leading to occlusion of these vessels. Perhaps, the most common is that described by Dajee et al. in the first known recorded case of acute aortic occlusion following a seat belt injury. They proposed that a circumferential tear of the intima leads to dissection and prolapse of the inner aortic layers, causing complete luminal occlusion [8].
Most acute occlusions are evident within 24 h, and delayed presentations are uncommon. The paediatric population have a greater capacity for the development of collaterals. As such, patients may remain asymptomatic until a period of growth spurt or they resume more rigorous physical activity. This can lead to delay in the diagnosis, and a high index of suspicion needs to be maintained to avoid ischaemic complications such as limb length discrepancy [8, 9]. The initial presentation may simply be that of extra-arterial haematoma. In such instances, it is important to rule out any secondary occlusion of the femoral artery and vein that may predispose to the development of thrombosis within these vessels. Duplex sonography should be carried out to assess flow velocities and waveform characteristics in these patients, and is especially suited to the paediatric population as they have reduced abdominal fat, and there is no radiation. In addition, a study by Fry et al. [10] identified ultrasound, in the right hands, to be highly sensitive (100%) and specific (97.5%) for the detection of arterial injuries when compared with surgical findings.
Open arterial thromboendarterectomy with graft or patch repair is the standard of care for such cases in trauma centres [10]. Previously documented cases include patch repair or bypass using saphenous vein, bovine pericardium and synthetic material [1–3, 5, 6]. One case was successfully treated with IV heparinzation alone [7]. However, in most injuries, the presence of significant groin haematoma may limit anticoagulation, requiring more urgent operative re-vascularization. In our patient, delayed presentation and presence of significant collaterals meant definitive operative management could be planned as a semi-elective procedure. The role of endovascular intervention in this paediatric population has previously been documented mainly as a temporizing measure for revascularization [4, 5]. Angiletta et al. [4] used a nitinol stent in the distal superficial femoral artery of a 13-year-old patient whose arterial and venous calibre at the time of injury were of inappropriate size for reconstruction. The main disadvantage of endovascular interventions in paediatric patients is the constantly enlarging calibre of the vessel with a fixed stent diameter. This can predispose to complications such as restenosis, stent fracture, stent dislocation and acute on chronic ischaemia [4]. As a result, future vascular reconstruction may be compromised and in extreme cases, this may progress to significant ischaemia and even limb loss. We provide an unusual cause of external iliac occlusion secondary to bicycle handlebar injury to the groin. All patients presenting with groin injury from this mechanism should be carefully investigated with duplex sonography and monitored for risk of vascular injury. The presence of collaterals, particularly in the paediatric population, can lead to delay in diagnosis. Literature seems to advocate open primary surgery for management of these injuries; however, endovascular and conservative medical management have also been used successfully. The latter two were contraindicated in our patient and open surgery was the most appropriate option. Long-term follow-up, beyond the 12-month period, is needed, particularly in relation to known vascular complications including pseudoaneurysms, arteriovenous fistula formation and restenosis.
CONFLICT OF INTEREST STATEMENT
None declared.



