-
PDF
- Split View
-
Views
-
Cite
Cite
Nicolae Crisan, Cristina S. Ivan, Catalina Bungardean, Cristina Cebotaru, Ioan Coman, Retroperitoneal perirenal myxoid liposarcoma, Journal of Surgical Case Reports, Volume 2015, Issue 3, March 2015, rju127, https://doi.org/10.1093/jscr/rju127
Close - Share Icon Share
Abstract
Liposarcomas are neoplasms of mesodermic origin, are derived from adipose tissue and represent <1% of all malignant tumours. Primary liposarcomas of the kidney are very rare. Here, we present the cases of two patients diagnosed with retroperitoneal perirenal myxoid liposarcoma. The patients were diagnosed via imaging, which in both cases revealed a huge right retroperitoneal tumour mass compressing the abdominal organs and large blood vessels. Surgical intervention consisting of en bloc resection of the tumour and the right kidney was performed using a transperitoneal approach. Three years after the surgery, both patients presented local recurrence, for which they underwent chemotherapy. Liposarcomas with renal origin are rare clinical entities with a high rate of malignancy and a poor prognosis. Because the use of chemotherapy and radiotherapy in the treatment of such liposarcomas is controversial, the treatment of choice is wide surgical resection with clean margins.
INTRODUCTION
Retroperitoneal liposarcomas represent a rare subtype of soft tissue sarcoma because of their localization (only 20% of soft tissue sarcomas are located retroperitoneally) and histological type (only 15% of soft tissue sarcomas are liposarcomas and, of these, only a third develop from perirenal fat) [1, 2]. The disease is more frequent in men in the fifth decade of life and has non-specific symptoms induced by the tumour [2].
CASE REPORT
Here, we present the cases of two patients, of different ages, diagnosed with perirenal myxoid liposarcoma.
The first is the case of a 65-year-old man without significant personal history who presented to the general practitioner with a progressively distended abdomen associated with weight loss, fatigue and dyspnoea. Abdominal ultrasonography and contrast-enhanced abdominal computed tomography (CT) found a voluminous, mixed-density mass located retroperitoneally in the right perirenal area; the mass was approximately 39 × 39 × 38 cm in size, with clearly defined, irregular margins and a few visible vessels, and was subsequently identified macroscopically as a right renal angiomyolipoma. The mass was in contact with the pancreas (displacing the cephalic and corporeal sides of the pancreas), the stomach (the distal third), the aorta, the liver (the visceral side), the gallbladder, the ascending and transverse colon, the inferior vena cava and the portal vein. The mass occupied the entire right hemi-abdomen, compressing the abdominal organs, displacing the liver cranially above the sixth rib and compressing the large vessels (Fig. 1). Thoracic CT revealed the presence of pulmonary emboli (Fig. 2), for which we initiated specific therapy.

Thoracic and abdominal CT—right perirenal retroperitoneal liposarcoma with massive secondary thromboembolism.
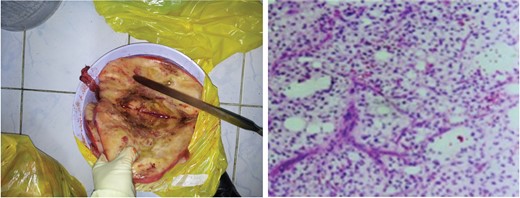
Perirenal myxoid liposarcoma—macroscopic appearance (left) and microscopic appearance (right).
After the haemodynamic status of the patient was optimized, surgical intervention was performed via a transperitoneal approach, and a retroperitoneal mass weighing 14 kg was excised. During surgery, no metastases were found in other abdominal organs, so no other organ resection was necessary. The operating time was 250 min, and 3 units of ABO/D group-compatible blood were administered.
Pathological examination revealed elements of perirenal myxoid liposarcoma, Fédération Nationale des Centres de Lutte Contre le Cancer (FNCLCC) Grade 2 (score 2 + 1 + 1 = 4), without lymphatic or vascular invasion and with negative resection margins.
Adjuvant therapy was administered after surgery according to the INNO-206 protocol as follows: INNO-206 was administered at 350 mg/m2 (260 mg/m2 doxorubicin equivalent) intravenously on Day 1 every 21 days for up to six consecutive cycles. The patient was monitored by thoracic and abdominal CT at 3, 6 and 12 months after surgery. Local recurrence was identified at the 18-month check-up, and the patient was started on chemotherapy with duloxetine at 30 mg/day for the first week and 60 mg/day for the next 4 weeks.
The second case was of a 70-year-old male patient who presented with abdominal pain. Contrast-enhanced CT revealed, in the retroperitoneal right perirenal area, a mass measuring 20 × 22 × 27 cm in size, of mixed structure including predominantly fluid and fatty components. The mass displaced the right kidney and the ascending colon towards the midline. The surgical procedure chosen was en bloc excision of the mass together with the right kidney via a transperitoneal approach. Histopathological examination revealed elements suggestive of an FNCLCC Grade 2 (score 4) myxoid liposarcoma derived from perirenal fat (pT2bN0M0L0V0R0). The patient was monitored via CT and, 3 years after the surgery, presented a local recurrence, for which he required chemotherapy.
DISCUSSION
Retroperitoneal perirenal liposarcomas are rare tumoural entities that are highly aggressive and have a poor prognosis. Since they develop in the retroperitoneal space, initially with asymptomatic progression, their diagnosis is frequently delayed until they are large, and they are difficult to treat.
Sixty percent of retroperitoneal liposarcomas measure >10 cm at the time of diagnosis; thus, early diagnosis and treatment of perirenal liposarcomas remain challenging. Most authors report local recurrence in the first 2 years after surgery, sometimes at multiple sites, even in cases with well-differentiated histology [3, 4]. Both our reported patients had local recurrence—even the patient diagnosed at the local stage (the second).
Retroperitoneal liposarcomas contain adipocytes of various sizes, and lipoblasts, and these cells are suspended in an intensely vascularized myxoid matrix. The mitotic index in these tumours is high, thus producing areas of acute ischaemic necrosis, and focal areas which can be described as sclerosing liposarcomas [5]. Some histological types also include an osteosarcoma-like or clear renal cell component [1], but we have not encountered those types in our experience. High-grade liposarcomas have an aggressive evolution with systemic dissemination, especially to the lungs, so the majority of patients have a low survival rate after surgical intervention.
Several factors are known to correlate with recurrence or survival, such as age over 50 years, advanced tumoural stage, incomplete tumoural resection, poor tumour differentiation, infiltration of resection margins, lymph node infiltration and the presence of metastases [2]. Treatment involves resection of the tumoural mass en bloc, with adjacent organ resection when needed. The positive margin rate in one large series, either macroscopically or microscopically, was 51%, and the efficacy of radiotherapy or chemotherapy in these cases remains controversial [3].
CONFLICT OF INTEREST STATEMENT
None declared.



