-
PDF
- Split View
-
Views
-
Cite
Cite
Cem Basatac, Mehmet Cagatay Cicek, Vesicocutaneous fistula treatment by using omental flap interposition, Journal of Surgical Case Reports, Volume 2015, Issue 2, February 2015, rjv004, https://doi.org/10.1093/jscr/rjv004
Close - Share Icon Share
Abstract
A fistula is defined as an abnormal association of two or more epithelial lining. Therefore, vesicocutaneous fistula (VCF) represents an extra anatomic communication between the bladder wall and the external surface of the skin. The most common cause is iatrogenic; however, numerous factors may play a role in the formation of VCFs. When a VCF is identified, it should be treated properly due to its bothersome complaints and social effects. Nonetheless, no certain consensus has been achieved, yet. In this case, we report the feasibility and efficacy of omental flap interposition during VCF repair.
INTRODUCTION
It is well known that vesicocutaneous fistulae (VCFs) result in uncontrollable urine leakage from the bladder to the skin. It causes bothersome complaints and dramatically impairs patients' quality of life. Most of these fistulae are iatrogenic, but this condition can also be caused by extensive trauma with pelvic fractures, postoperative causes of radical pelvic surgery, after irradiation of pelvic malignancies, hip arthroplasty and large bladder calculus, and other different etiologic causes have been also reported [1–4]. In addition, untreated VCF leads to continuous wetness and odor. As a result, when VCF is recognized, it should be treated properly. However, there is no consensus regarding the treatment of this situation, yet. Simple repair with tissue approximation is often difficult because of the extent of tissue destruction and cicatrization. Since VCFs are usually referred as complex fistulae, interposition grafts or flaps can be used to enhance repair of the fistula tract. Nevertheless, surrounding tissue may not be suitable for this procedure due to severe inflammation, radiation and fibrosis. In this study, we present a case of VCF treated with omental flap interposition.
CASE REPORT
A 32-year-old male presented to our outpatient clinic with complaints of dysuria and continuous leakage of urine from the fistula tract located at the midpoint of the symphysis pubis and the umbilicus for a long time. In his medical history, he underwent open surgery due to a large bladder stone at 24 years of age. A nontender mass was palpable around the orifice on physical examination. The urinalysis revealed pyuria and microscopic hematuria, but the urine culture was sterile. An abdominal ultrasonography was done, but no remarkable pathology was reported. A computerized tomography (CT) cystogram demonstrated an aberrant connection between the anterior bladder wall and the external surface of the skin (Fig. 1A). Subsequently, under general anesthesia, patient was placed in a low lithotomy position. Cystoscopy was performed to visualize and cannulate the fistula tract with a 6-Fr ureteral catheter. A midline infraumblical incision was made involving the circumscribing incision around the fistula. The fistula tract was identified until the bladder with blunt dissection. After excision of fistula tract with wide perivesical tissue debridement, a peritoneal cavity was opened and an omental V-shaped flap was prepared (Fig. 2A). An omental flap was based on a more reliable right gastroepiploic artery and brought down to the surgical field and placed upon the anterior bladder wall. The omental flap was sutured and quilted on the bed of the anterior bladder wall with the interrupted 2-0 polyglactin sutures (Fig. 2B). The border of the suture lines included from the bladder neck to the posterior bladder wall and up to endopelvic fascia at the lateral sides. A closed pelvic drain was also placed. No intraoperative and postoperative complications were noted. The drain was removed day after surgery, and the patient was discharged at the postoperative day 2. A Foley catheter was removed at the postoperative day 21 after a CT cystogram revealed no leakage from the bladder (Fig. 1B). At the last follow-up visit, patient was relieved of all his complaints.
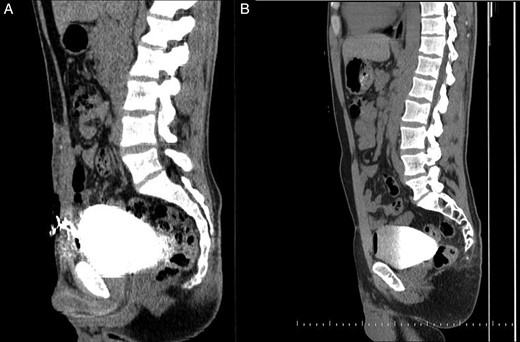
(A) A CT cystogram demonstrates an aberrant connection between the anterior bladder wall and the external surface of the skin. (B) A CT cystogram shows no leakage from the bladder on postoperative day 21.
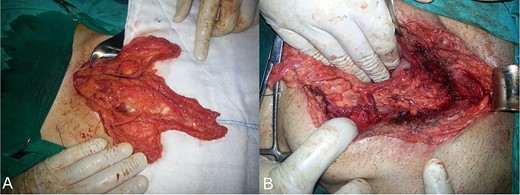
(A) An omental V-shaped flap prepared to enhance repair of VCFs. (B) An omental flap was sutured and quilted on the bed of the anterior bladder wall.
DISCUSSION
After cutaneous fistulous tracts are excised and bladder defects are closed, attention is turned to cover suture lines with graft or flap interposition over the bladder to anchor securely to the site of fistula. Myocutaneous rectus abdominis grafts should be considered primarily [5]. These grafts can be used based on the inferior epigastric arterial pedicle for the repair of VCF. However, myocutaneous grafts sometimes may not be available because of dens adjacent tissue fibrosis and severe inflammation. In this context, the omentum may be an acceptable alternative. Interposition of an omental flap during VCF repair does not only add an extra layer to the VCF repair to prevent recurrence, but also increases lymphatic drainage and decreases the risk of infected fluid collection. The use of omental flap in urinary tract fistula repair was first described by Kiricuta and Goldstein in 1972 [6]. Since then, numerous studies have demonstrated feasibility of omental flap with considerable success rates [7]. Orford and Theron [8] successfully repaired 52 patients with vesicovaginal fistulae (VVFs) by means of omental flap interposition and reported a 93% cure rate. Evans et al. reported 29 patients who underwent transabdominal VVF repair with or without omental flap. Ten patients in whom omental flap was used were successful (100%). Nevertheless, only 12 of the remaining 19 patients who did not receive omental flap were cured (63%). Because of this reason, the authors concluded that omental flap should be routinely used during transabdominal VVF repair even in benign fistulas with well-preserved surrounding tissue [9]. Though omentum most commonly has been used as an interpositional layer between the bladder and vagina during transabdominal VVF repair, data are lacking in the literature whether omental flap would be efficacious in the repair of VCF. Lau and Cheng [2] have shown a favorable result with omental flap interposition in their case of VCF that occurred after radiation therapy. As in this case, when the surrounding tissues do not appear healthy and well vascularized, omental V-shaped flap based on the right gastroepiploic artery may be a suitable alternative to reduce recurrence. This report may encourage the use of omental flap when the surrounding tissue is not appropriate. In conclusion, interposition of omental flap during the treatment of VCF can be a suitable and feasible alternative because of its rich vascular and lymphatic supply, together with its resistance to infection, when the surrounding tissue is not available. However, high-volume and comparative studies are needed so as to determine optimal treatment modality in this condition.
CONFLICT OF INTEREST STATEMENT
None declared.



