-
PDF
- Split View
-
Views
-
Cite
Cite
Clarissa Nóbrega Gambarra Nascimento, Robson Luis Amorim, Maurício Mandel, Marcelo Prudente do Espírito Santo, Wellingson Silva Paiva, Almir Ferreira Andrade, Manoel Jacobsen Teixeira, Endoscopic-assisted removal of traumatic brain hemorrhage: case report and technical note, Journal of Surgical Case Reports, Volume 2015, Issue 11, November 2015, rjv132, https://doi.org/10.1093/jscr/rjv132
Close - Share Icon Share
Abstract
The endoscopic technique has been described as a minimally invasive method for spontaneous hematoma evacuation, as a safe and effective treatment. Nevertheless, to our knowledge, there is no description of a technical report of traumatic intracerebral hematoma removal using the neuroendoscope. A 47-year-old man was admitted sustaining 13 points in Glasgow coma scale with brain computed tomography (CT) scan showing a temporal contusion. Guided by a 3D reconstructed CT, using the program OsiriX®, the posterior limit of the hematoma was identified. A burr hole was placed at the posterior temporal region, and we used the neuroendoscope to assist the hematoma evacuation. The postoperative tomography showed adequate hematoma removal. He was discharged from hospital 48 h after surgery. Two weeks later, he was conscious and oriented temporally. This endoscopic-assisted technique can provide safe removal of traumatic hematomas of the temporal lobe.
INTRODUCTION
Minimally invasive approaches have been the actual goal for neurosurgery. In line with this philosophy, spontaneous intracerebral hemorrhage has been treated by neuroendoscopy since 2003. The technique was first described under stereotactic guidance, showing promising results.
Besides the esthetic benefit of the minimally invasive approach, there is the possibility to minimalize the operative time and length of hospital stay. At an emergency setting, these principles are strongly useful. Nevertheless, there is no description of traumatic hematoma evacuation using such technique.
CASE REPORT
A 47-year-old patient was admitted with a Glasgow coma scale (GCS) of 13 points and remained neurologically stable until surgery, which he was submitted after 72 h of trauma. Although he was neurologically stable, the location of the hematoma implicated in the risk of brain stem compression with normal intracranial pressure. It would be necessary to observe for a long period to be sure that there were no more risks for the hematoma expansion.
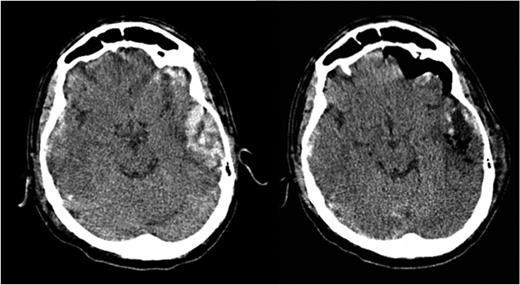
Brain computed tomography (CT) scan showed a temporal hematoma with 30 ml of volume, extending from the temporal posterior region to the anterior compartment of the right media fossa. The volume and the location of the hematoma implicate in a high risk of brain stein compression.
The brain CT scan was reconstructed using the program OsiriX, as shown in Fig. 1, so that it was possible to establish accurate cranial landmarks to guide the burr hole position.
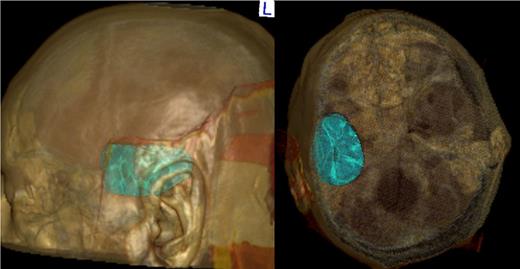
After the patient was put in the proper position, guided by the 3D imaging, we were able to perform a single small incision and a single burr hole at the posterior aspect of the hematoma. The neuroendoscope (Storz–HOPKINS®–Forward–Oblique Telescope 30°) was positioned in a 45° direction, headed from the posterior limit of the hematoma to the media fossa floor, in a way that the whole hematoma could be visualized. With the neuroendoscope in place, the surgeon uses the other hand to hold a 7–9 gauge suctor. Then, both the suctor and the neuroendoscope are progressively inserted through the burr hole, following the natural corridor provided by the hematoma evacuation. After satisfactory hematoma evacuation, the camera was again placed to confirm hemostasis. If some level of hemorrhage emerges, irrigation with 0.9% saline is enough to stop bleeding. If bleeding persists, pieces of surgicel can be left in place. A small piece of Gelfoam is placed over the burr hole, and the wound is closed in layers.
The patient was discharged from hospital after 48 h of surgery. The comparison between the pre- and postoperative CT scans is shown in Fig. 2.
DISCUSSION
In the actual scenario of minimally invasive techniques, the endoscopic method has been at high spot, especially for intracerebral hematomas. In contrast, for hemorrhagic strokes several authors, with or without complementary methods, have described the technique.
In 2010 [1] was described a similar technique to the one used in this report. The author used a 3D reconstructed CT scan to guide the entry point, depth of penetrating path and surgical trajectory. An intraoperative sonography was also used for confirmation. The average hematoma evacuation rate was 82%.
Using stereotactic guidance [2] described a hematoma evacuation inserting the endoscopy through a metal tube positioned by stereotaxic. The holder assured that the guide tube did not move, providing safety to the procedure.
Other papers [3–5] confirm that the method is safe with lower mortality compared with the conventional method to treat spontaneous hematomas, and those do not extend the operative time. In traumatic brain injuries, these features may decrease the operative time, which is crucial for a safer procedure. When considering posterior fossa, it is marked the time gained with the endoscopic technique (64.5 versus 230.6 min), as described by Yamamoto T. [6].
Considering these advantages, two groups applied the endoscopic technique for acute subdural hematomas drainage [7, 8] describing one case of non-traumatic and other traumatic large acute subdural hematomas. The patients were 86 and 87 years old, both with good neurological recovery.
The technical note presented in this report expresses the tendency of minimally invasive surgeries, focused on lower operative time and lower blood loss, besides the esthetic aspect considered as another advantage.
Endoscopic surgery, usually described for spontaneous hematomas, may expend its perspectives considering the reduced time of surgery, blood loss and safety, and may also be considered for traumatic brain injuries.
This case report is the first to describe the endoscopic technique applied to traumatic intracranial hematoma. Also, comparing it to the other tools described before to guide the procedure, the surgical planning reported here has the great advantage that does not require any cost and is also simple to use. Our group has already described the use of the open access Osirix software for planning craniotomy or burr hole in the emergency setting with a detailed description on how to use the tools provided by the software [9], which surely does not postpone the procedure. Nevertheless, its use to assist an endoscopic surgery was not described in our previous article.
This first described technique could be widely spread considering its cost and all the possible morbidities that could be applied, gathering both safety and effectiveness for minimally invasive procedures.
CONFLICT OF INTEREST STATEMENT
None declared.



