-
PDF
- Split View
-
Views
-
Cite
Cite
Gwion Daniel, Robert Coleman, Staged rotation flap scrotoplasty and orchidopexy in a patient with inguinal ectopic scrotum, Journal of Surgical Case Reports, Volume 2015, Issue 10, October 2015, rjv137, https://doi.org/10.1093/jscr/rjv137
Close - Share Icon Share
Abstract
Ectopic scrotum is a rare and unusual presentation to paediatric urology. It is usually characterized by accessory scrotum with adequate scrotum in the anatomically normal position. We describe a case of inguinal ectopia of the right hemiscrotum containing the right testis, and its staged surgical management by rotation flap scrotoplasty and subsequent orchidopexy.
INTRODUCTION
Ectopic scrotum is a rare condition, which has been described as affecting either side, and may or may not contain testis [1–3]. Hoar et al. demonstrated that when described, it is frequently associated with other genitourinary congenital abnormalities [1]. We describe our staged surgical management of a child with right ectopic scrotum and testis by flap scrotoplasty with subsequent orchidopexy after 6 months.
CASE REPORT
A 5-month-old boy born at 36 weeks gestation was referred to our tertiary institution from primary care with an undescended right testis and right-sided scrotal skin tag. Ultrasound and MAG3 scans had previously demonstrated a solitary left kidney. He was otherwise well and thriving, with growth noted to be in the 25th centile at a recent paediatrician review.
Initial assessment revealed ectopia of virtually the entire right hemiscrotum, which was located in the inguinal region and contained the right testis. The left side of his scrotum had developed in its normal position and contained the left testis. The ectopic scrotal skin had a small central skin tag. There was intervening normal skin between the two halves of his scrotum.
He was again reviewed at 1 year of age and planned for elective surgery to correct position of the ectopic scrotum with subsequent orchidopexy 6 months later.
He underwent rotation flap correction of right ectopic scrotum with paediatric urology and plastic surgery input. Skin perforator blood vessels were identified using a Doppler ultrasound, allowing the position and size of the skin flaps to be planned. The ectopic scrotal skin was pedicled superiorly with an inferior pedicle to the intervening skin. Flaps were mobilized with perforator vessel preservation and switched. Skin was closed with interrupted subcuticular 5-0 biosyn. The testicle was left in its original inguinal location. At post-operative follow-up of 2 weeks, the wound was healing well, and the flap had entirely survived.
Right orchidopexy was undertaken 6 months later with excision of the skin tag and the testis placed in a dartos pouch within the repositioned scrotum.
At outpatient follow-up, the repositioned scrotum had an excellent cosmetic appearance and contained a viable right testis, comparable in size with that on the left.
DISCUSSION
Congenital abnormalities of the scrotum are rare with few reported cases in the literature [4]. Ectopic scrotum describes the anomalous position of scrotal tissue and can be suprainguinal, infrainguinal or perineal [5]. In many of the reported cases of patients with suprainguinal ectopic scrotum, there are associated upper urinary tract abnormalities, particularly ipsilateral renal agenesis [1–3, 5] and renal dysplasia [2, 5]. It has been recommended that patients with an ectopic scrotum should undergo ultrasonography to image the upper urinary tract [4].
After the onset of sexual differentiation at the end of the seventh week of foetal development, the urogenital sinus opens on the surface of the perineum. The genital tubercle is a midline swelling that grows at the cephalic end. Posterior to this, a urethral fold forms on either side of the urogenital membrane. Labial swellings then form lateral to each of the urethral folds. The testes ultimately descend into the labial swellings, which become distended and move medially to form the scrotum by fusion of each labial fold, forming the median scrotal raphe.
Testicular descent from the lumbar area to the labioscrotal folds is by a complex mechanism. The cranial suspensory ligament is a fibromuscular structure anchoring the embryonic gonad to the posterior abdominal wall; its regression permits testicular descent [6]. It is thought that loss of the cranial suspensory ligament in males is dependent on testosterone, secreted along with Müllerian inhibiting substance (MIS) by the developing testis [7]. MIS causes regression of the Müllerian ducts, preventing formation of fallopian tubes, uterus and the upper vagina.
The role of the caudal genital ligament, more commonly known as the gubernaculum in the descent of the testis, has been described in detail as far back as 1956 [8]. It was so named ‘pilot’ by John Hunter in the 18th century because of his belief that it steered the testis to the scrotum [7]. It is a band of tissue that extends from the labioscrotal fold through the inguinal canal and onto the body of the testis and its epididymis. In normal development, the gubernaculum grows into a thick cord and guides the testis into its final position in the scrotum. Swelling of the distal gubernaculum during the transabdominal phase makes the ligament short and fat, which anchors it to the future inguinal canal. This produces relative descent of the testis against the enlarging abdominal cavity [9]. The inguinoscrotal phase of testicular descent requires the gubernaculum to extend across the pubis and into the scrotum in the perineum. Intra-abdominal pressure plays a supplementary role in the inguinoscrotal phase of descent, as a result of the processus vaginalis, a diverticulum of peritoneum contained within the gubernaculum [10].
The role of the gubernaculum in testicular descent is not yet fully understood [10], but Hoar et al. state that it is a prerequisite for the final location of both the testis and the scrotum [1]. Embryological basis for scrotal ectopia is unknown; however, a defect in gubernacular development or function may prevent migration of the labioscrotal swellings, resulting in ectopic scrotum [1].
Management of ectopic scrotum using a scrotal rotation flap and subsequent orchidopexy (Fig. 1) has not been previously described. Excision of accessory ectopic scrotal tissue is appropriate when adequate orthotopic scrotum is present to accommodate the testis [4]. When the entire hemiscrotum is ectopic, pedicled flap rotation of the ectopic scrotal skin with subsequent orchidopexy is a safe surgical approach with excellent cosmetic and functional results (Figs 2 and 3).

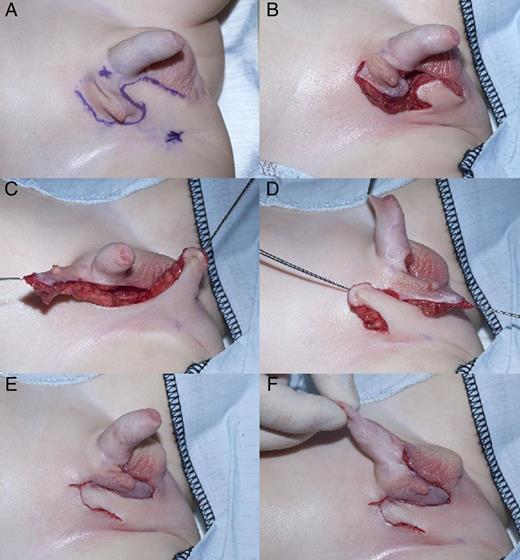
Rotation flap correction of ectopic scrotum: (A) marked flaps and perforator vessels, (B) raised flaps, (C and D) flaps rotated and (E and F) skin closure.

CONFLICT OF INTEREST STATEMENT
None declared.



