-
PDF
- Split View
-
Views
-
Cite
Cite
Shahin Hajibandeh, Shahab Hajibandeh, Michelle Johnpulle, Vittorio Perricone, Transperitoneal repair of a juxtarenal abdominal aortic aneurysm and co-existent horseshoe kidney with division of the renal isthmus, Journal of Surgical Case Reports, Volume 2015, Issue 10, October 2015, rjv134, https://doi.org/10.1093/jscr/rjv134
Close - Share Icon Share
Abstract
The co-existence of abdominal aortic aneurysm (AAA) and horseshoe kidney (HSK) is rare. We report a 67-year-old man with an expanding juxtarenal AAA associated with a HSK. The aneurysm had a severely angulated neck and contained a significant amount of mural thrombus. The isthmus of HSK closely lied over the aneurysm, making its exposure extremely difficult. The aneurysm was successfully repaired using transperitoneal approach with division of the renal isthmus and without any need for the renal artery reconstruction. Despite the potential complications, particularly renal insufficiency, associated with division of the renal isthmus and suprarenal cross-clamping of the abdominal aorta, in our case, post-operative period was uneventful and the patient's recovery was satisfactory.
INTRODUCTION
Horseshoe kidney (HSK) is the most common congenital abnormality of the kidney, occurring in 0.15–0.25% of newborns, with a male-to-female ratio of 2:1 [1]. HSK is characterized by three anatomical anomalies: ectopia, malrotation and changes in vascular supply [2]. Fusion is usually at the lower poles resulting in the kidneys been caught at the level of the developing inferior mesenteric artery [2, 3]. The isthmus that connects the lower renal poles in HSK may either be a fibrous band or contain functional parenchymal tissue [4].
The co-existence of abdominal aortic aneurysm (AAA) and HSK is rare, occurring only in 0.12% of patients [5]. The isthmus in HSK almost always lies over the aneurysm, making its exposure extremely difficult [6]. Moreover, the complex anatomical anomalies of the kidney and of its collecting system and arteries make the surgical repair of the aneurysm very challenging [3]. Therefore, accurate preoperative imaging is required in order to design appropriate surgical strategy.
We report a rare case of juxtarenal AAA associated with HSK, which was successfully repaired using transperitoneal approach with division of the renal isthmus.
CASE REPORT
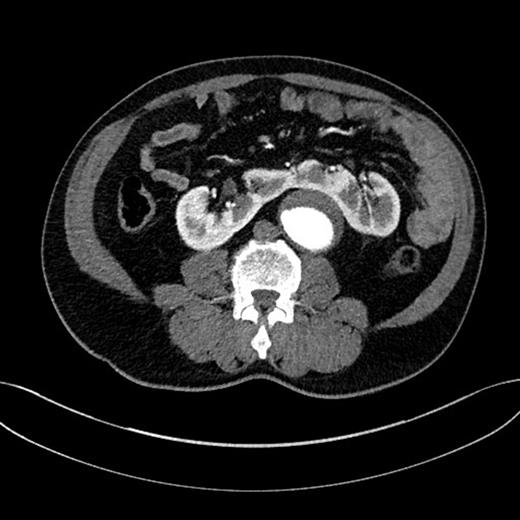
A 67-year-old man, with a known AAA of 4.42 cm, was found to have expansion of the aneurysm diameter to 5.40 cm after undergoing a 3-month surveillance ultrasound scan. The patient's aneurysm was further investigated by a computed tomography angiography (CTA), which demonstrated a 5.50 cm juxtarenal AAA that was not suitable for endovascular AAA repair (EVAR) because of a severely angulated proximal neck. The aneurysm contained a significant amount of mural thrombus. Moreover, the CTA demonstrated a HSK anterior to the abdominal aorta (Fig. 1). Following a multidisciplinary team discussion, an open repair with involvement of both vascular and urology surgeons was decided.
Using a transperitoneal approach, we identified a juxtarenal AAA and a HSK with both renal pelvises located medially. The renal isthmus closely lied over the aneurysm, and there was a small vein draining blood from the renal isthmus to the left renal vein, but no accessory artery supplying the renal isthmus was found (Fig. 2). Both ureters were identified and preserved. The left renal artery was identified and dissected free from the proximal neck of the aneurysm. Provisional clamping of the left renal artery resulted in ischaemia of the left kidney and the renal isthmus, indicating that the arterial blood supply of the renal isthmus was from the left renal artery. Considering the minimal gap between the aneurysm and the renal isthmus, we had concerns over controlling retrograde lumbar bleeding when the aneurysm is open; therefore, we decided to divide the renal isthmus in order to facilitate exposure of the aneurysm. The left renal vein was preserved, and the vein draining the renal isthmus was divided and ligated. Careful division of the renal isthmus over the aneurysm was carried out, and homeostasis was achieved.
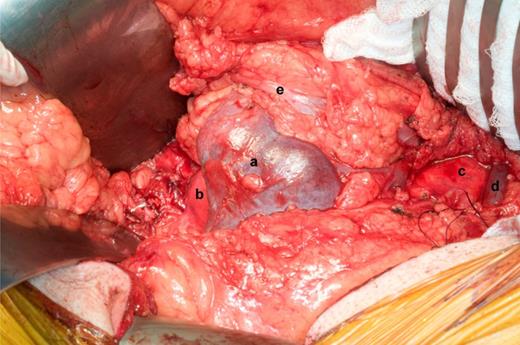
(a) HSK (the isthmus), (b) the distal segment of aneurysm close to the iliac bifurcation, (c) the aneurysm neck, (d) the left renal vein and (e) the left ureter.
Suprarenal clamp over the left renal artery was applied for 22 min. The aneurysm was repaired using a 20 mm Dacron without the left renal artery reconstruction (the graft was sutured obliquely so that the origin of the left renal artery was patent) (Fig. 3).
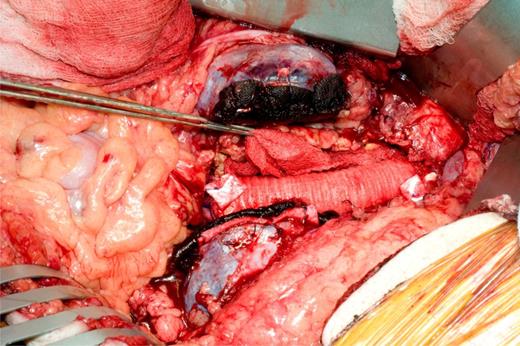
The divided renal isthmus and repaired aneurysm using a 20 mm Dacron.
The post-operative recovery was uneventful, and the patient had stable renal function. The patient was mobile on Day 3 after the operation and was discharged with good condition on Post-operative Day 5. Out-patient follow-up of the patient was satisfactory.
DISCUSSION
The co-existence of AAA and HSK is rare [5]. Several surgical approaches have been used to repair AAA in patients with co-existent HSK. Transperitoneal approach provides the best exposure to the aneurysm and kidney, however, the presence of the renal isthmus affects both surgical exposure and proximal aortic control [7]. Left retroperitoneal approach has the advantage of avoiding interference with the renal isthmus and urinary tracts; however, access to the right iliac artery is limited [7]. In our case, the endovascular approach was not suitable because the proximal neck of the aneurysm was severely angulated.
Division of the renal isthmus can be associated with increased risk of retroperitoneal urinary leaks, bleeding, infection and renal ischaemia [6]. Connelly et al. [8] demonstrated successful division of the renal isthmus in 24 patients with AAA and co-existent HSK without any post-operative renal necrosis or urine leaks. However, they did not recommend routine division of the renal isthmus but did not hesitate to advise the division of the isthmus when it facilitates the operation. In our case, we had to divide the renal isthmus to facilitate exposure of the aneurysm. In fact, considering the substantial difficulty in exposing the aneurysm due to overlying isthmus, we had concerns over controlling retrograde lumbar bleeding when the aneurysm is open.
Suprarenal cross-clamping, especially if it is for longer than 30 min, has been shown to increase the serum creatinine by itself to >200 µmol/l regardless of the presence or absence of anatomic malformations [9,10]. We had to use suprarenal cross-clamping (over the left renal artery only) for 22 min, which did not increase the post-operative creatinine significantly (118 µmol/l). However, it should be taken into account that our patient had normal renal function before the operation, while an abnormal preoperative renal function is known to be an important indicator of poor prognosis in patients with AAA and co-existent HSK [9,10]. Moreover, we did not have to perform the renal artery reconstruction, which is often necessary in patients with AAA and co-existent HSK when temporary renal exclusion takes place [3]. In fact, we avoided the left renal artery reconstruction by suturing the graft obliquely at the origin of the left renal artery.
We reported a rare case of juxtarenal AAA associated with HSK, which was successfully repaired using transperitoneal approach with division of the renal isthmus. Despite the potential complications, particularly renal insufficiency, associated with division of the renal isthmus and suprarenal cross-clamping of the abdominal aorta, in our case, post-operative period was uneventful and the patient's recovery was satisfactory.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
Author notes
S. H. and S. H. have equally contributed to this paper and joined first authorship is proposed.



