-
PDF
- Split View
-
Views
-
Cite
Cite
Fahad Jamil, Khalid Hussain, Vocal cord palsy as a presenting feature of sternoclavicular joint septic arthritis, Journal of Surgical Case Reports, Volume 2015, Issue 1, January 2015, rju147, https://doi.org/10.1093/jscr/rju147
Close - Share Icon Share
Abstract
Sternoclavicular joint septic arthritis (SSA) is rare and often difficult to manage condition. The sternoclavicular joint is an unusual site of septic arthritis in healthy persons, but may be commonly involved in intravenous drug users, primary or secondary immunosuppressive disorders, infections or the presence of infected central lines. After thorough literature search, no cases have yet been reported on SSA leading to vocal cord palsy. The following case describes a male patient who presented to hospital with left vocal cord palsy and symptoms consistent with aero-digestive tract malignancy. Radiological examination and subsequent response to treatment demonstrated the only causative pathology to be an ipsilateral septic sternoclavicular joint.
INTRODUCTION
Sternoclavicular joint septic arthritis (SSA) and its clinical presentation are infrequently seen and often difficult to manage. Presenting symptoms of SSA can vary, with chest and shoulder pain being the most common clinical features. Other presenting complaints include neck pain and swelling over the sternoclavicular joint area. After thorough literature search, no cases have yet been reported on SSA leading to vocal cord palsy.
Vocal cord palsy is an important sign of thoracic and head and neck pathology that is caused by an extremely wide set of pathology. This case has shown SSA to be a causative factor for vocal cord palsy.
CASE REPORT
A 67-year-old gentleman presented to the emergency department with a 3-week history of worsening dysphagia and hoarse voice. His past medical history includes hypercholestrolaemia, osteoarthritis and hypertension only. He is an ex-smoker of 20 years. Routine examination of the patient in the emergency department revealed that he was haemodynamically stable and apyrexial and exhibited tenderness in the left anterior neck. Examination by the otolaryngology team demonstrated no evidence of cervical lymphadenopathy but tenderness of the lower left anterior triangle, as well as evident swelling, erythema and mild bruising of the anterior chest wall. On questioning the patient regarding this, he revealed that he burnt his chest using a hot water bottle ∼3 weeks previously and he also admitted to having stiffness and pain in the left shoulder over this same period. Indirect laryngoscopy with flexible nasendoscopy revealed non-discrete swelling/oedema of the left pharayngeal wall and reduced mobility of the left vocal cord. Routine haematological investigation revealed a white cell count of 18.6 × 109/l, C-reactive protein of 288 mg/l and platelets of 499 × 109/l. No other haematological abnormality was noted on admission.
With a working differential of parapharyngeal space infection and possible malignancy, the patient was referred for a computed tomography (CT) scan of the neck and thorax with contrast. The patient was also started empirically on intravenous co-amoxiclav as treatment for neck space collection. CT imaging, performed 24 h after admission, revealed no evidence of malignancy or indeed any paraphayrngeal space collection. Few small lymph nodes were noted on the left side of the neck, but were deemed to be reactive in nature, and left vocal cord palsy was evident (Fig. 1). The key finding was that of a left sternoclavicular joint collection and closely associated superficial anterior chest wall, soft tissue swelling and oedema (Fig. 2). This inflammatory process was also noted deep to the manubrium and sternum and extending somewhat into the mediastinum with evident enlarged mediastinal lymph nodes (Fig. 3). The CT findings were in keeping with SSA with associated superficial and deep tissue inflammation and oedema. With no other cause found, the vocal cord palsy was attributed to the inflammation within the mediastinum, which in turn was caused by superficial burn from hot water bottle use.
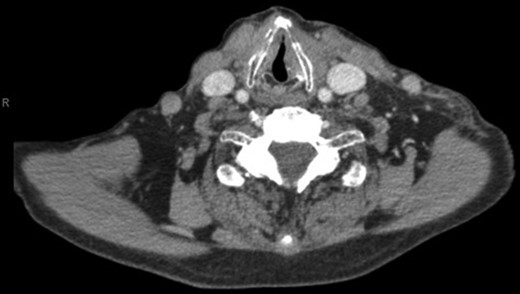
Computed tomography. A 67-year-old male with SSA. Findings: left vocal cord palsy indicated by the para-median position of the left vocal cord in comparison with the right. Technique: contrast-enhanced axial CT of the neck and thorax.

Computed tomography. A 67-year-old male with SSA. Findings: left sternoclavicular joint collection and closely associated superficial anterior chest wall, soft tissue swelling and oedema. The oedema can be seen to be spreading into the chest. Technique: contrast-enhanced axial CT of the neck and thorax.
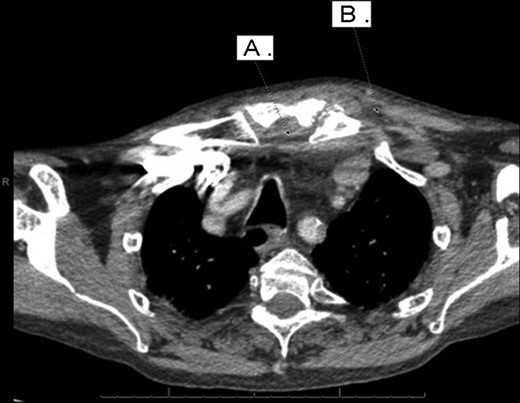
Computed tomography. A 67-year-old male with SSA. Findings: soft tissue oedema of the chest seen retrosternally (marker A) and superficially on the left anterior chest (marker B) as well as evidence of mediastinal lymph node enlargement. Technique: contrast-enhanced axial CT of the neck and thorax.
The antibiotic regimen for the patient was converted to intravenous benzylpenicillin (1.2 g four times per day) and flucloxacillin (1 g four times per day). Response to antibiotic therapy was limited in the first few days of admission with little change in haematological inflammatory markers. After discussion with the microbiologist, the flucloxacillin was increased to 2 g four times a day on the fourth day of admission. The patient made slow but positive improvements over the course of the next 8 days while on intravenous antibiotics, after which he was successfully discharged. He continued on oral antibiotics and on outpatient review 3 weeks after his admission, his external swelling, erythema and voice had returned to normal. Repeat CT performed 3 months following discharge demonstrated complete resolution of the deep and superficial inflammatory process as well as the mediastinal lymph nodes.
DISCUSSION
Vocal cord palsy can be due to weakness in one or both vocal cords, and diagnosis is made when reduced mobility is evident by laryngoscope examination. In a review of 117 cases, Benninger et al. [1] attributed the following as the most common causes of vocal cord palsy: surgical trauma (44%), malignancies (17%), endotracheal intubation (15%), neurological disease (12%) and idiopathic causes (12%). No correlation between SSA and vocal cord palsy has yet been documented. Furthermore, a review of 389 vocal cord palsy cases by Holinger et al. [2] makes no reference to the cause being related to a septic sternoclavicular joint.
Explanations for this unusual presentation of SSA seen in this case include tracking infection from the septic sternoclavicular joint, resulting in a vocal cord palsy due to reactive mediastinal lymphadenopathy. Spreading infectious sequeale of SSA have been well documented and include empyema, osteomyelitis and mediastinitis [3]. Significant contributing factors to these outcomes are the methicillin-resistant Staphylococcus aureus (MRSA) strains, which are becoming increasingly prevalent [4]. A literature review of 180 cases shows mediastinitis as a clinical feature in up to 13% of patients with SSA [5]. However, the direct link between mediastinitis and vocal cord palsy is less clear. Reports of fibrosing mediastinitis and descending necrotizing mediastinitis leading to vocal cord palsy have been documented [6]. The mild reactive mediastinal inflammation seen in the presented case has not been presented in the literature as a cause of vocal cord palsy. Therefore, as mentioned previously, it is most likely explained by mediastinal lymphadenopathy, which is a known cause of left vocal cord palsy in malignancy and atypical infections such as tuberculosis [7].
It has been shown that if radiological findings indicate a limited extent of disease, then medical therapy alone should be sufficient. This empirical antibiotic coverage should be active against S. aureus, the most common infective agent in SSA [8]. Joint resection would only be indicated if extensive bony destruction, chest wall phlegmon or abscess, retrosternal abscess, mediastinitis or pleural extension is evident on CT/MRI imaging [9]. It is clear from the haematological and radiological findings, as well as the response to treatment, that all the presenting features of this patient were as a result of the septic focus in the sternoclavicular joint.
CONFLICT OF INTEREST STATEMENT
None declared.



