-
PDF
- Split View
-
Views
-
Cite
Cite
Qing Ting Tan, Esther Wee Lee Chuwa, Sung Hock Chew, Ga Sze Hong, Schwannoma: an unexpected diagnosis from a breast lump, Journal of Surgical Case Reports, Volume 2014, Issue 9, September 2014, rju085, https://doi.org/10.1093/jscr/rju085
Close - Share Icon Share
Abstract
Schwannomas or neurilemmomas are benign neoplasms of the Schwann cells in neural sheaths. They may arise in any nerve in the body and occur frequently in the head and neck region or extremities. While breast lumps and schwannomas are very common, mammary schwannomas are exceedingly scarce with <30 cases reported in the literature. We describe a case of a breast schwannoma in a 37-year-old female and review the literature surrounding this rare occurrence.
INTRODUCTION
Schwannomas are the most common peripheral nerve tumours. These benign slow-growing neoplasms originate from Schwann cells which form myelin in peripheral nerves. They tend to favour nerves in the head and neck region as well as nerves in the upper and lower extremities. Schwannomas in the breast, however, are extremely rare. We report such a case in a patient who presented with a breast lump, initially presumed to have a phyllodes tumour.
CASE REPORT
A 37-year-old Chinese female presented with a lump in the left breast that was slowly growing over a duration of 8 years. Aside from a history of amenoblastoma of the jaw which was excised 3 years ago, she has no significant medical history. On physical examination a firm 1-cm nodule was palpable at the 3 o'clock position of the left breast. Mammography showed a well-circumscribed opacity in the left breast (Fig. 1) and ultrasound revealed an ovoid 1.5 × 1.5 × 0.9 cm heterogeneous solid hypoechoic nodule with well-defined, regular margins (Fig. 2). The lesion contained some anechoic areas suggestive of cystic clefts which are consistent with sonographic features of a phyllodes tumour [1, 2].
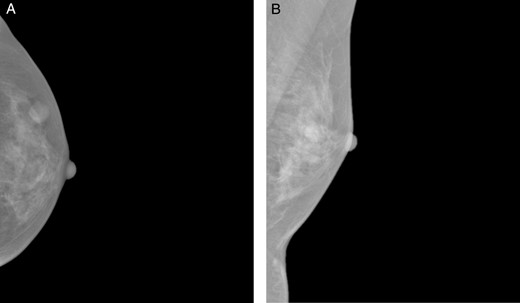
Craniocaudal (A) and mediolateral oblique (B) mammographic views demonstrating a well-circumscribed opacity in the central outer quadrant of the left breast.

Sonographic views of an ovoid well-marginated nodule containing some cystic clefts. This lesion was initially thought to represent a phyllodes tumour.
Our patient underwent an excisional biopsy without a preoperative needle biopsy. A 1.2 × 1.2 × 0.8 cm smooth well-encapsulated nodule was removed in entirety from the breast parenchyma. On bisection, the cut section displayed a pale pink smooth homogeneous appearance. Microscopic evaluation showed an encapsulated spindle cell tumour with prominent nuclear palisading and features typical of a schwannoma (Fig. 3). There was also strong and diffuse positive staining of S-100, favouring the diagnosis of schwannoma (Fig. 4). There was no evidence of malignancy in the specimen.
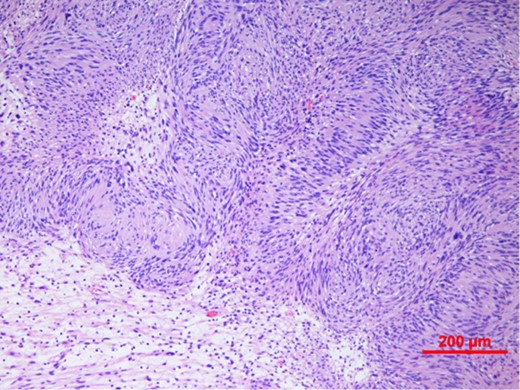
Spindle cell tumour with palisaded arrangement of nuclei, typical of schwannoma. Cellular (Antoni A) areas alternate with looser myxoid (Antoni B) areas.
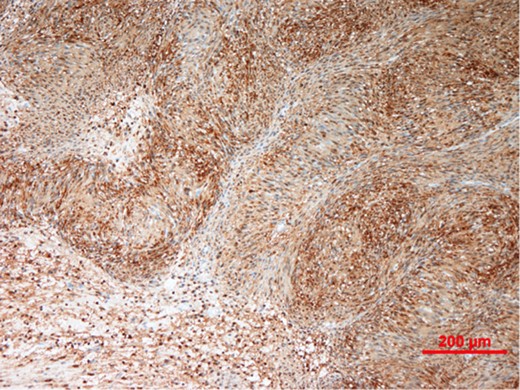
Immunohistochemistry showing tumour cells staining strongly and diffusely for S-100 protein.
DISCUSSION
Schwannomas or neurilemomas or neurinomas are the most common peripheral nerve tumours. They commonly affect young adults, usually in the third decade of life. These slow-growing neoplasms arise from Schwann cells, which produce the insulating myelin sheath in peripheral nerves. They are mostly benign tumours that tend to favour nerves in the head and neck as well as the extremities [3–6]. While schwannomas may occur in any part of the body, they are extremely rare in the breast. A review of the literature shows only 28 cases of benign breast schwannomas (Table 1) [3–7]. Schwannomas tend to occur as solitary well-encapsulated masses. Sizes of the masses range from 0.7 to 11 cm with a mean and median size of 3.7 and 3 cm, respectively. Before histological correlation, breast schwannomas tend to be mistaken for a range of pathologies ranging from benign fibroadenomas to cancer.
| Author . | Age . | Sex . | Symptom . | Duration of symptom . | Size (cm) . | Test performed . | Preoperative diagnosis . | ||
|---|---|---|---|---|---|---|---|---|---|
| US . | MMG . | FNAC . | |||||||
| Collins [3] | 43 | F | Lump | 10 days | 2.0 | Fibroadenoma | |||
| Majmudar [3] | 18 | F | Lump | 9 months | 2.5 | Fibroadenoma | |||
| Van der Walt [3] | 38 | F | Lump | NS | 3.0 | Cancer | |||
| 39 | F | Lump | NS | 0.8 | NS | ||||
| Krishnan [3] | 43 | F | Lump | 6 months | 3.0 | Cancer | |||
| Harrison [3] | 24 | F | Lump | 2 years | 6.0 | NS | |||
| Cohen [3] | 80 | F | Lump | NS | 9.0 | Yes | NS | ||
| 75 | M | NS | NS | 9.0 | NS | ||||
| 20 | F | NS | NS | 2.8 | NS | ||||
| NS | F | NS | NS | 1.0 | NS | ||||
| Martinez-Onsurbe [3] | 83 | M | Lump | 6 months | 4.0 | Yes | Gynecomastia | ||
| Bernardello [3] | 18 | F | Lump | 6 months | 1.0 | Yes | Yes | Yes | Mesenchymal neoplasm |
| Tokita [3] | 62 | F | Pain | 1 month | 1.5 | Yes | Yes | Intracystic papilloma | |
| Gultekin [3] | 50 | F | Mass on MMG | NS | 0.7 | Yes | NS | ||
| Mondal [3] | 38 | M | Lump | 9 months | 3.5 | Yes | Schwannoma, adenoma | ||
| 56 | M | Lump | 2 years | 8.6 | Yes | Schwannoma | |||
| 74 | M | Lump | 1 year | 11.0 | Yes | Schwannoma | |||
| Galant [3] | 25 | F | 2 Lumps | 8 months | 3.0, 1.6 | Yes | Yes | Yes | Mesenchymal spindle cell tumour |
| Gupta [3] | 35 | M | Lump | 4 weeks | 2.0 | Yes | Schwannoma | ||
| 56 | F | Lump | 2 weeks | 3.0 | Yes | Schwannoma | |||
| Cho [6] | 76 | F | Lump | 9 months | 1.2 | Yes | Yes | NS | |
| Tohnosu [3] | 64 | F | Lump | 1 day | 2.3 | Yes | Yes | Yes | Fibroadenoma |
| Uchida [3] | 45 | F | Lump | 4 years | 3.2 | Yes | Yes | Yes | Phyllodes tumor |
| Rashidi [3] | 27 | F | Lump | NS | 7.0 | Yes | Yes | NS | |
| Lee [5] | 41 | F | Lump | 10 years | 7.0 | Yes | Yes | Cancer | |
| Bellezza [3] | 58 | F | Lump | 7 months | 4.4 | Yes | Yes | Yes | Mesenchymal neoplasm |
| Balci [7] | 61 | F | Mass on MMG | NS | 1.2 | Yes | Yes | NS | |
| Dialani [4] | 64 | F | Mass on MMG | NS | 1.0 | Yes | Yes | NS | |
| Our case | 37 | F | Lump | 8 years | 1.2 | Yes | Yes | Phyllodes tumor | |
| Author . | Age . | Sex . | Symptom . | Duration of symptom . | Size (cm) . | Test performed . | Preoperative diagnosis . | ||
|---|---|---|---|---|---|---|---|---|---|
| US . | MMG . | FNAC . | |||||||
| Collins [3] | 43 | F | Lump | 10 days | 2.0 | Fibroadenoma | |||
| Majmudar [3] | 18 | F | Lump | 9 months | 2.5 | Fibroadenoma | |||
| Van der Walt [3] | 38 | F | Lump | NS | 3.0 | Cancer | |||
| 39 | F | Lump | NS | 0.8 | NS | ||||
| Krishnan [3] | 43 | F | Lump | 6 months | 3.0 | Cancer | |||
| Harrison [3] | 24 | F | Lump | 2 years | 6.0 | NS | |||
| Cohen [3] | 80 | F | Lump | NS | 9.0 | Yes | NS | ||
| 75 | M | NS | NS | 9.0 | NS | ||||
| 20 | F | NS | NS | 2.8 | NS | ||||
| NS | F | NS | NS | 1.0 | NS | ||||
| Martinez-Onsurbe [3] | 83 | M | Lump | 6 months | 4.0 | Yes | Gynecomastia | ||
| Bernardello [3] | 18 | F | Lump | 6 months | 1.0 | Yes | Yes | Yes | Mesenchymal neoplasm |
| Tokita [3] | 62 | F | Pain | 1 month | 1.5 | Yes | Yes | Intracystic papilloma | |
| Gultekin [3] | 50 | F | Mass on MMG | NS | 0.7 | Yes | NS | ||
| Mondal [3] | 38 | M | Lump | 9 months | 3.5 | Yes | Schwannoma, adenoma | ||
| 56 | M | Lump | 2 years | 8.6 | Yes | Schwannoma | |||
| 74 | M | Lump | 1 year | 11.0 | Yes | Schwannoma | |||
| Galant [3] | 25 | F | 2 Lumps | 8 months | 3.0, 1.6 | Yes | Yes | Yes | Mesenchymal spindle cell tumour |
| Gupta [3] | 35 | M | Lump | 4 weeks | 2.0 | Yes | Schwannoma | ||
| 56 | F | Lump | 2 weeks | 3.0 | Yes | Schwannoma | |||
| Cho [6] | 76 | F | Lump | 9 months | 1.2 | Yes | Yes | NS | |
| Tohnosu [3] | 64 | F | Lump | 1 day | 2.3 | Yes | Yes | Yes | Fibroadenoma |
| Uchida [3] | 45 | F | Lump | 4 years | 3.2 | Yes | Yes | Yes | Phyllodes tumor |
| Rashidi [3] | 27 | F | Lump | NS | 7.0 | Yes | Yes | NS | |
| Lee [5] | 41 | F | Lump | 10 years | 7.0 | Yes | Yes | Cancer | |
| Bellezza [3] | 58 | F | Lump | 7 months | 4.4 | Yes | Yes | Yes | Mesenchymal neoplasm |
| Balci [7] | 61 | F | Mass on MMG | NS | 1.2 | Yes | Yes | NS | |
| Dialani [4] | 64 | F | Mass on MMG | NS | 1.0 | Yes | Yes | NS | |
| Our case | 37 | F | Lump | 8 years | 1.2 | Yes | Yes | Phyllodes tumor | |
US, ultrasonography; MMG, mammography; FNAC, fine needle aspiration cytology; NS, not specified.
| Author . | Age . | Sex . | Symptom . | Duration of symptom . | Size (cm) . | Test performed . | Preoperative diagnosis . | ||
|---|---|---|---|---|---|---|---|---|---|
| US . | MMG . | FNAC . | |||||||
| Collins [3] | 43 | F | Lump | 10 days | 2.0 | Fibroadenoma | |||
| Majmudar [3] | 18 | F | Lump | 9 months | 2.5 | Fibroadenoma | |||
| Van der Walt [3] | 38 | F | Lump | NS | 3.0 | Cancer | |||
| 39 | F | Lump | NS | 0.8 | NS | ||||
| Krishnan [3] | 43 | F | Lump | 6 months | 3.0 | Cancer | |||
| Harrison [3] | 24 | F | Lump | 2 years | 6.0 | NS | |||
| Cohen [3] | 80 | F | Lump | NS | 9.0 | Yes | NS | ||
| 75 | M | NS | NS | 9.0 | NS | ||||
| 20 | F | NS | NS | 2.8 | NS | ||||
| NS | F | NS | NS | 1.0 | NS | ||||
| Martinez-Onsurbe [3] | 83 | M | Lump | 6 months | 4.0 | Yes | Gynecomastia | ||
| Bernardello [3] | 18 | F | Lump | 6 months | 1.0 | Yes | Yes | Yes | Mesenchymal neoplasm |
| Tokita [3] | 62 | F | Pain | 1 month | 1.5 | Yes | Yes | Intracystic papilloma | |
| Gultekin [3] | 50 | F | Mass on MMG | NS | 0.7 | Yes | NS | ||
| Mondal [3] | 38 | M | Lump | 9 months | 3.5 | Yes | Schwannoma, adenoma | ||
| 56 | M | Lump | 2 years | 8.6 | Yes | Schwannoma | |||
| 74 | M | Lump | 1 year | 11.0 | Yes | Schwannoma | |||
| Galant [3] | 25 | F | 2 Lumps | 8 months | 3.0, 1.6 | Yes | Yes | Yes | Mesenchymal spindle cell tumour |
| Gupta [3] | 35 | M | Lump | 4 weeks | 2.0 | Yes | Schwannoma | ||
| 56 | F | Lump | 2 weeks | 3.0 | Yes | Schwannoma | |||
| Cho [6] | 76 | F | Lump | 9 months | 1.2 | Yes | Yes | NS | |
| Tohnosu [3] | 64 | F | Lump | 1 day | 2.3 | Yes | Yes | Yes | Fibroadenoma |
| Uchida [3] | 45 | F | Lump | 4 years | 3.2 | Yes | Yes | Yes | Phyllodes tumor |
| Rashidi [3] | 27 | F | Lump | NS | 7.0 | Yes | Yes | NS | |
| Lee [5] | 41 | F | Lump | 10 years | 7.0 | Yes | Yes | Cancer | |
| Bellezza [3] | 58 | F | Lump | 7 months | 4.4 | Yes | Yes | Yes | Mesenchymal neoplasm |
| Balci [7] | 61 | F | Mass on MMG | NS | 1.2 | Yes | Yes | NS | |
| Dialani [4] | 64 | F | Mass on MMG | NS | 1.0 | Yes | Yes | NS | |
| Our case | 37 | F | Lump | 8 years | 1.2 | Yes | Yes | Phyllodes tumor | |
| Author . | Age . | Sex . | Symptom . | Duration of symptom . | Size (cm) . | Test performed . | Preoperative diagnosis . | ||
|---|---|---|---|---|---|---|---|---|---|
| US . | MMG . | FNAC . | |||||||
| Collins [3] | 43 | F | Lump | 10 days | 2.0 | Fibroadenoma | |||
| Majmudar [3] | 18 | F | Lump | 9 months | 2.5 | Fibroadenoma | |||
| Van der Walt [3] | 38 | F | Lump | NS | 3.0 | Cancer | |||
| 39 | F | Lump | NS | 0.8 | NS | ||||
| Krishnan [3] | 43 | F | Lump | 6 months | 3.0 | Cancer | |||
| Harrison [3] | 24 | F | Lump | 2 years | 6.0 | NS | |||
| Cohen [3] | 80 | F | Lump | NS | 9.0 | Yes | NS | ||
| 75 | M | NS | NS | 9.0 | NS | ||||
| 20 | F | NS | NS | 2.8 | NS | ||||
| NS | F | NS | NS | 1.0 | NS | ||||
| Martinez-Onsurbe [3] | 83 | M | Lump | 6 months | 4.0 | Yes | Gynecomastia | ||
| Bernardello [3] | 18 | F | Lump | 6 months | 1.0 | Yes | Yes | Yes | Mesenchymal neoplasm |
| Tokita [3] | 62 | F | Pain | 1 month | 1.5 | Yes | Yes | Intracystic papilloma | |
| Gultekin [3] | 50 | F | Mass on MMG | NS | 0.7 | Yes | NS | ||
| Mondal [3] | 38 | M | Lump | 9 months | 3.5 | Yes | Schwannoma, adenoma | ||
| 56 | M | Lump | 2 years | 8.6 | Yes | Schwannoma | |||
| 74 | M | Lump | 1 year | 11.0 | Yes | Schwannoma | |||
| Galant [3] | 25 | F | 2 Lumps | 8 months | 3.0, 1.6 | Yes | Yes | Yes | Mesenchymal spindle cell tumour |
| Gupta [3] | 35 | M | Lump | 4 weeks | 2.0 | Yes | Schwannoma | ||
| 56 | F | Lump | 2 weeks | 3.0 | Yes | Schwannoma | |||
| Cho [6] | 76 | F | Lump | 9 months | 1.2 | Yes | Yes | NS | |
| Tohnosu [3] | 64 | F | Lump | 1 day | 2.3 | Yes | Yes | Yes | Fibroadenoma |
| Uchida [3] | 45 | F | Lump | 4 years | 3.2 | Yes | Yes | Yes | Phyllodes tumor |
| Rashidi [3] | 27 | F | Lump | NS | 7.0 | Yes | Yes | NS | |
| Lee [5] | 41 | F | Lump | 10 years | 7.0 | Yes | Yes | Cancer | |
| Bellezza [3] | 58 | F | Lump | 7 months | 4.4 | Yes | Yes | Yes | Mesenchymal neoplasm |
| Balci [7] | 61 | F | Mass on MMG | NS | 1.2 | Yes | Yes | NS | |
| Dialani [4] | 64 | F | Mass on MMG | NS | 1.0 | Yes | Yes | NS | |
| Our case | 37 | F | Lump | 8 years | 1.2 | Yes | Yes | Phyllodes tumor | |
US, ultrasonography; MMG, mammography; FNAC, fine needle aspiration cytology; NS, not specified.
Although schwannomas frequently occur in young adults, cases reported to have an age range from 18 to 83 years with a mean age of 48.6 and a median age of 45. Six of the 28 (21.4%) reported cases occurred in males [3].
On mammography, most schwannomas appear as well-circumscribed opacities. In certain cases, they may be mammographically occult or may present as ill-defined soft tissue densities [3]. Sonographically, they are generally described as well-defined hypoechoic lesions. Other features suggestive of a schwannoma on ultrasound include target sign (hyperechoic centre and hypoechoic periphery), posterior acoustic enhancement and peripheral nerve continuity. However, these features may also represent other peripheral nerve sheath tumours like neurofibromas [8]. The mass in our patient had cystic areas which were also reported by Lee [5] and Uchida [3].
Macroscopically, breast schwannomas are described as white, grey, tan or pink well-encapsulated masses. Microscopically, they are spindle cell tumours with Antoni A patterns (hypercellular areas with palisading nuclei surrounding pink areas called Verocay bodies) and Antoni B patterns (hypocelluar regions with looser stroma and myxoid change) Schwannomas almost always stain positive for S100 protein. A cytologic diagnosis via fine needle aspiration may be possible if clusters of spindle-shaped cells arranged in a palisading fashion and lacking epithelial elements are seen [3].
To the best of our knowledge, there has been no report documenting the diagnosis of schwannoma via a core needle biopsy. This might be useful as a larger sample would be available for microscopic evaluation compared with fine needle aspiration cytology, possibly avoiding open excision to confirm its benign histology. With the increase in clinically occult image-detected lesions [3, 4, 7], small lesions may be amenable to complete excision by large-bore vacuum-assisted biopsy devices with both diagnostic and therapeutic intent.
26% of malignant schwannomas occur in patients with neurofibromatosis [9]. There have been only four reports of malignant schwannomas arising in the breast with Malas [10] reporting the only case of malignant schwannoma of the breast in a woman with neurofibromatosis. The diagnosis of malignant schwannoma was only achieved post-operatively in the four cases. Sonographically, the masses can appear benign and fine needle aspiration cytology has not been helpful in discerning a malignant schwannoma from other mesenchymal tumours [3].
Schwannomas occurring in the breast are very rare and frequently mistaken for a range of benign to malignant lesions such as fibroadenomas, phyllodes tumour, mesenchymal neoplasms or even breast epithelial cancers. They are largely benign slow-growing lesions and in the absence of distinguishing features on radiology or cytology, a non-operative mode of diagnosis such as a core needle biopsy or large-bore vacuum-assisted biopsy might be considered. In patients with neurofibromatosis where the risk of malignancy within a schwannoma is higher, MRI may be helpful in detecting suspicious lesions for biopsy.



