-
PDF
- Split View
-
Views
-
Cite
Cite
Paras K. Pandove, Ashish Moudgil, Megha Pandove, Kamna Aggarwal, Divya Sharda, Vijay K. Sharda, Multiple ileal perforations and concomitant cholecystitis with gall bladder gangrene as complication of typhoid fever, Journal of Surgical Case Reports, Volume 2014, Issue 7, July 2014, rju070, https://doi.org/10.1093/jscr/rju070
Close - Share Icon Share
Abstract
Surgical complications of typhoid fever usually involve the small gut, but infrequently typhoid fever also involves the gallbladder. Complications range from acalculous cholecystitis, gangrene to perforation. Here, we present a case of enteric fever with concomitant complication of multiple ileal perforations at its terminal part with acalculous cholecystistis with gangrenous gall bladder. The primary closure of the perforations and cholecystectomy was performed. Post-operatively patient developed low-output faecal fistula that was managed conservatively.
INTRODUCTION
Typhoid fever is a common infection that has continued to be a public health problem in many developing countries, particularly in areas with poor sanitation and limited availability of clean, potable water. The World Health Organization (WHO) conservatively puts the annual global incidence of typhoid fever at 21 million cases, with 1–4% mortality [1]. The disease predominantly affects school-age children (5–15 years of age), although it does occur in younger children [1]. Surgical complications of typhoid usually involve the small gut rather than the gallbladder and Salmonella typhi is more common than S. parathyphi [2]. In the gut, it commonly causes intestinal perforation, resulting in high morbidity and mortality. It rarely causes acute cholecystitis, gangrene or perforation of the gall bladder. When these two complications coexist mortality rate is increased.
CASE REPORT
A 14-year-old female was admitted to our ward with a 12–15 days history of fever. She had a 4-day history of severe abdominal pain with abdominal distension and obstipation for 3 days. On examination, she was febrile with pulse rate 118/min, BP 90/60 mmHg and tachypnoea, which were suggestive of septicaemic shock. She had abdominal distension with rigidity and absent bowel sounds. Chest X-ray revealed air under the diaphragm and ultrasound abdomen showed a large amount of free fluid with internal echoes in all peritoneal recesses. Provisional diagnosis of enteric perforation peritonitis was made and patient taken up for exploratory laparotomy after resuscitation and routine investigations. The abdomen was full of free fluid and pus with faecal smell. Pus for culture sensitivity sent. Inspection of bowel revealed multiple perforations of the ileum at an antimesentric border, one near ileocaecal junction and two in its proximal part (Fig. 1 and 2 ) along with oedematous, distended gangrenous gall bladder with inflammation and oedema of the adjacent structures (Fig. 3) associated with congestion and inflammation of whole of the small gut. The primary closure of all the perforations after biopsy was done along with cholecystectomy. The abdomen closed in layers over drains after proper toilet. The Widal test was positive with titres of anti-O 1 : 160 and anti-H titres 1 : 160. Pus C/S showed growth of Escherichia coli and appropriate antibiotics given.
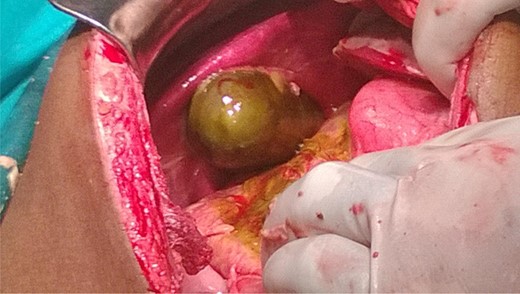
Gangrenous gall bladder with inflamed and oedematous surrounding structures.
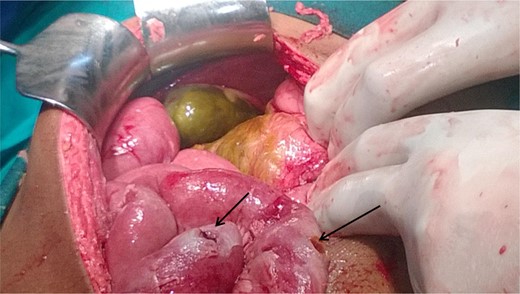
Showing gangrenous gall bladder and two ileal perforations (arrows marked).
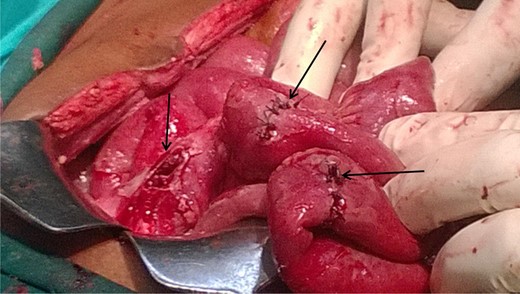
Three ileal perforations (arrows marked), two repaired and one to be repaired.
Histopathology of the perforations revealed inflammation and of gall bladder showed acalculous cholecystitis. Post-operatively patient developed faecal fistula that was managed conservatively.
DISCUSSION
Typhoid fever is a common cause of enteric perforation classically occurring in the ileum in the second week of illness [2]. Children account for >50% of all cases of typhoid intestinal perforation, with a peak age incidence of 5–9 years affecting boys and girls equally. The overall perforation rate of typhoid in children is ∼10%, but the perforation rate appears to increase with age, reaching a high of 30% by 12 years of age [3].
Most common causes of acute cholecystitis are infection and cholelithiasis, but ∼2–15% of cases are acalculous cholecystitis, with mortality rates ranging from 6 to 67% [4]. Typhoid complicated by cholecystitis has a reported incidence of 2.8 with 1.7% being acalculous [5].
In 1915, Lothrop [6] reported the first case of acute acalculous cholecystitis as a complication of typhoid fever. Typhoid fever may either be a primary or secondary event leading to acute acalculous cholecystitis. Routes of gallbladder infection by typhoid bacilli may be either through blood stream, biliary system or contiguous infected organs or lymphatics from gastrointestinal tract [7].
The pathophysiology of acalculous cholecystitis complicating typhoid fever is incompletely defined. Endotoxin-mediated injury seen in gram-negative sepsis is one of the proposed mechanism. These mediators lead finally to biliary stasis that results in increased bile viscosity, sludge formation and increases the gallbladder mucosal damage [8]. In turn, these mechanisms often result in functional or secondary mechanical obstruction of the cystic duct from inflammation. Another proposed mechanism includes abnormal permeability of serous membranes and capillary leakage as a result of direct invasion of the gallbladder wall by typhoid bacilli, resulting in gallbladder distension and wall thickening.
In only 2–30% of patients, the disease progresses to gangrenous cholecystitis with wall perforation, which may occur due to persistent occlusion of the cystic duct by the presence of an impacted stone, increased gall bladder wall tension, epithelial injury, release of phospholipases, degradation of adjacent cell membranes and intense inflammatory reaction [9]. Fundus of the gallbladder is the most distal site of vascular supply and most common site for perforation [10]. The combination of enteric perforation with gall bladder perforation in typhoid fever increases the mortality manifold. Acute typhoidal acalculous cholecystitis may be managed conservatively with antibiotics. The complicated ones, i.e. gangrenous cholecystitis, perforation,chronic carrier state or relapse are managed with cholecystectomy [2].
In 2007, a case was reported with multiple ileal perforations in enteric fever for which re-section anastomosis was done. On the fourth post-operative day pain abdomen with distension and bilious wound discharge led to re-exploration which revealed gall bladder perforation and cholecystectomy was performed [2].
Typhoid fever with multiple ileal perforations and concomitant gall bladder gangrene has probably not been reported before in the literature as present in our case. A little delay in presentation or exploration could have led to perforation of the gall bladder. The purpose of presenting such case is to stress upon associated or isolated gall bladder complications, though rare in cases of enteric fever. Thus, it necessitates routine examination of the gall bladder in cases of enteric fever gut perforations to rule out associated gall bladder complications at laparotomy which if present carries high morbidity and mortality rate. Early interventions can reduce the associated mortality.



