-
PDF
- Split View
-
Views
-
Cite
Cite
C.R. Shaw, J. Badhesha, G. Ayana, R. Abu-Rajab, Use of a proximal humeral plate for a paediatric peri-prosthetic femoral fracture, Journal of Surgical Case Reports, Volume 2014, Issue 7, July 2014, rju069, https://doi.org/10.1093/jscr/rju069
Close - Share Icon Share
Abstract
In this case an 18-year-old female with cerebral palsy sustained a peri-prosthetic femoral fracture adjacent to a blade plate previously inserted for a femoral varus osteotomy. The injury was treated using a long proximal humeral locking plate. The existing blade plate was removed. The fracture was reduced and held, and a 10-hole PHILOS™ plate applied with near anatomical reduction. There were no post-operative complications. Radiographic union was confirmed at 11 months. To our knowledge, this is the first reported use of a PHILOS™ plate in the management of a femoral peri-prosthetic fracture and successfully demonstrated a straightforward method for revision fixation.
INTRODUCTION
The AO-fixed-angle blade plate is popular among surgeons for fixation of proximal femoral osteotomies [1, 2] and is a common procedure for patients with significant hip displacement as a result of cerebral palsy. There are several complications associated after femoral osteotomy including wound infection, bursitis and peroneal nerve palsies, but fracture rates are relatively rare. This suggests little evidence is available to determine the best surgical management following a significant femoral fracture. The musculoskeletal difficulties commonly seen in quadriplegic cerebral palsy patients can add to the complexity of these cases, as younger patients may not be suitable for standard adult proximal femoral fixation techniques. We report a case of using of a proximal humeral plate for a revision fixation in a paediatric femoral fracture.
CASE REPORT
An 18-year-old female with a history of quadriplegic cerebral palsy (GMFCS-V) was admitted to our orthopaedic department following a peri-prosthetic fracture of the right femur. She is well known to our department, as her non-ambulatory status has resulted in a number of surgeries including a right adductor tenotomy, aged 11, femoral derotation osteotomy and dega acetabular osteotomy, aged 13 and right distal hamstring and knee capsule release, aged 14. She presented to the emergency department with a painful right thigh after getting her leg caught in doorway while being mobilized in a wheelchair. The trauma resulted in lateral bending of the leg, with examination revealing a significant deformity of the thigh with audible crepitus. Radiographs revealed a peri-prosthetic fracture of the right femoral shaft extending distal to the AO blade plate (Fig. 1). The blade was also seen to be encroaching on the inferior cortex of the femoral neck leading to concerns about creating a stress riser or femoral neck fracture in the event of revision blade plate fixation. There was also concern that the longest replacement blade plate available would not be of sufficient length to stabilize the fracture distally. The complexity of this case along with the patients low body weight (26 kg), small skeletal morphology and underlying neurological disorder deemed revision with a long-blade plate, or standard adult femoral fixation devices unsuitable. Therefore, we proposed a long PHILOS™ proximal humeral locking plate (Synthes, UK) as a suitable device for internal fixation of the fracture to provide adequate plate osteosynthesis, with secure proximal and distal fixation, bridging the fracture and the femoral neck defect.

AP-XR demonstrating a peri-prosthetic fracture of the right femur below the blade plate. Blade plate noted to be breaching femoral neck.
Under general anaesthesia, open reduction and internal fixation using a 10 hole philos plate was performed with the patient in a supine position on the traction table utilizing a lateral approach. Using C-arm image intensification, the height of the plate was judged, then applied to the bone and secured both proximally and distally to the fracture with proximal locking screws inserted where possible (Fig. 2a–c). Securing the cephalic segment of the philos plate to the proximal femur proved challenging due to the femoral neck defect left by the removal of the blade plate. Final reduction was judged to be near anatomical with the wound thoroughly irrigated with saline before closure. Post-operative treatment included IV antibiotics with mobility instructions unnecessary due to the patient's non-ambulatory status. The patient was discharged after 5 days with a follow-up period over 11 months. There were no post-operative complications during this time and radiographs showed an anatomically healed fracture (Fig. 3).
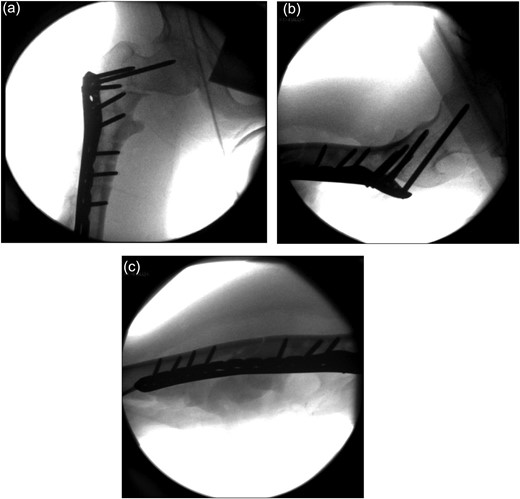
Image intensifier intra-operative AP highlighting 10 hole PHILOS applied with near anatomical reduction (a–c).

AP-XR demonstrating radiographic union at 11 months with 10 hole PHILOS insitu.
DISCUSSION
Peri-prosthetic fractures are relatively rare in paediatric populations with cerebral palsy. However, two studies have reported several fractures following proximal femoral osteotomies utilizing an AO-fixed-angle blade plate. The first of these studies by Beauchesne et al., [3] reported 14 various complications after performing proximal femoral osteotomies on a total of 157 paediatric patients. They reported only five fractures occurring in patients with cerebral palsy, with fractures of proximal fixation (two patients), distal plate fixation, proximal tibia and distal femur. Management of these fractures included cast immobilization, anterior plate and an interfragmentary screw with little comment found regarding the repair of the distal femur. Hau et al. [4] performed 58 femoral osteotomies utilizing an AO 90°-fixed-angle blade plate in children with cerebral palsy and noted only one fracture, which was revised using flexible intramedullary nails.
With the vast majority of femoral fractures treated by conservative means, little research has examined the best operative management of these patients. A number of difficulties can arise when considering management of femoral fractures in cerebral palsy (CP) patients, with previous studies having noted severity of contractures and non-ambulatory status impacting on higher malunion rates [5] and adding to the complexity of these cases. The few studies that have examined treatment of femoral fractures in CP patients have noted the majority of cases are treated conservatively, particularly in non-ambulaters [6]. Therefore, little is known of the most appropriate surgical management for patients unsuitable for long leg or spica cast application. To our knowledge only one retrospective study review exists that evaluated the treatment of femur fractures in both ambulators and non-ambulatory patients. Leet et al. [7] reported that although the majority of non-ambulators were treated conservatively at their centre, 6 of the 38 fractures were treated operatively, with procedures including percutaneous pinning, plate fixation, external fixation and intramedullary nailing.
To our knowledge, this is the first reported case of using a Philos plate (proximal humerus internal locking system) to treat a paediatric proximal femur fracture. The Philos plate is a locking compression plate that utilizes locking screws to provide stable fixation and hold in osteoporotic bone [8]. A number of studies have advocated its use in proximal humeral fractures, with encouraging evidence of both short- and long-term clinical outcomes [9, 10]. Although Philos plates have been exclusively designed for the treatment of proximal humerus fractures, this does not prevent their use at alternative sites. We found that application of a Philos plate provided a suitable alternative for stable fixation of a proximal femoral fracture with no long-term complications identified so far. It is important that trauma surgeons retain the ability for lateral thinking when approaching complex and challenging patients and fractures, though care should be taken when using implants in areas they were not specifically designed for.



