-
PDF
- Split View
-
Views
-
Cite
Cite
Jason Ramsingh, Ahmad Ali, Caroline Cameron, Ahmed Al-Ani, Robert Hodnett, Catriona Chorushyj, De Garengeot's hernia: diagnosis and surgical management of a rare type of femoral hernia, Journal of Surgical Case Reports, Volume 2014, Issue 2, February 2014, rju008, https://doi.org/10.1093/jscr/rju008
Close - Share Icon Share
Abstract
De Garengeot's hernia is quite rare and is a femoral hernia that contains a vermiform appendix and can present as a painful, tender swelling or an asymptomatic lump. We present the case of a 70-year-old patient who presented to our surgical unit after being referred for diagnostic imaging of an asymptomatic groin lump which was found to be a De Garengeot's hernia. She had an open repair of her femoral hernia and laparoscopic appendicectomy. Her post-operative stay was uneventful. De Garengeot's hernia is rare; however, imaging is usually required to make a diagnosis preoperatively. Management is usually surgical with simultaneous repair of the femoral hernia and appendicectomy.
INTRODUCTION
De Garengeot's hernia is quite rare and is defined as the presence of the vermiform appendix within a femoral hernia. It is often difficult to diagnose this condition preoperatively; however, the use of computed tomography (CT) scan can aid in the identification of this rare hernia and plan surgical management. We present the case of an elderly female who presented with an asymptomatic lump and required imaging to confirm the diagnosis. We also present the first documented combined open and laparoscopic approach for this rare entity.
CASE REPORT
A 70-year-old female was referred by her general practitioner to our radiology department after presenting with a painless right groin swelling. An ultrasound scan showed a lymph node in the right groin with surrounding fluid and unusual appearances not typical of a hernia. A limited CT scan was subsequently performed which revealed a right femoral hernia containing the tip of the vermiform appendix with surrounding inflammatory change and an associated enlarged lymph node in keeping with a De Garengeot's hernia (Figs 1–3). On questioning, the patient first noticed the lump 2 weeks prior to presentation and said that it has gradually increased in size. It was not painful and she had no obstructive symptoms. Her medical history included COPD, breast cancer and a past history of tuberculosis.
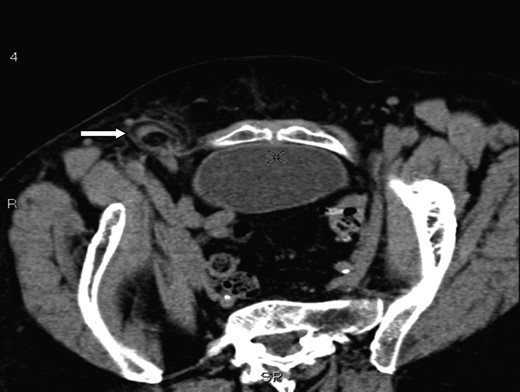
A axial section illustrating a right femoral hernia through the femoral canal at the level of pubic tubercle.
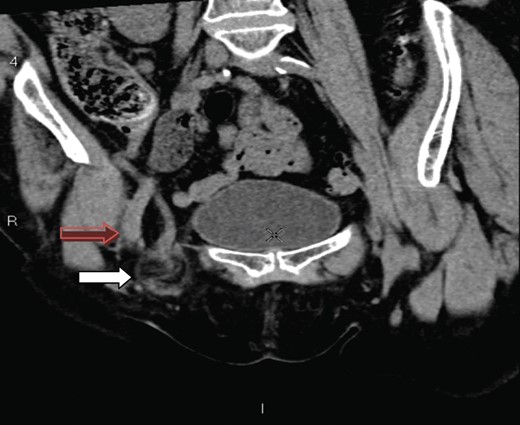
A coronal section showing the tip of the appendix (white arrow) protruding through the femoral canal, medial to femoral vein (red arrow) into the hernia. The appendix measures 10 cm.

A saggital section demonstrating the tip of the appendix (white arrow) within the femoral sac.
On examination, she was overweight and a non-tender swelling was palpable in her right groin. It was ∼4 cm in size, soft but not reducible and located below the groin crease. Bloods revealed a marginally elevated white cell count and CRP. She consented to an emergency open repair of her femoral hernia and appendicectomy. Her hernia was approached via a groin crease incision; however, it was difficult to dissect to the base of the appendix. A decision was made by the operating surgeon to complete her femoral repair using a mesh plug since the appendix appeared normal with no free fluid or inflammatory changes. Her appendix was removed laparascopically. Post-operatively, she recovered well and was discharged on the second day after her operation. Pathology report showed an acutely inflamed appendix.
DISCUSSION
In 1731, Rene Jacques Croissant de Garengeot was the first to describe the presence of a vermiform appendix within a femoral hernia [1]. This is a distinct entity from an appendix within an inguinal hernia as described by Claudius Amyand in 1735 [2]. The presence of a vermiform appendix within the femoral hernia is fortunately rare with an incidence rate of 5%, while an acute appendicitis within a groin hernia is even rarer with incidence rates of 0.1–0.5% [3, 4].
A review of 36 patients presenting with a de Garengeot's hernia found that 97% experienced a painful swelling [5]. Our patient presented with an asymptomatic groin swelling and required imaging to confirm the diagnosis of de Garengeot's hernia. CT scan was able to confirm the presence of an appendix within the femoral canal and is a useful tool in the evaluation of an asymptomatic groin swelling. Furthermore, this form of imaging can identify radiological findings of an inflamed appendix within a femoral canal as first published by Zissin et al. [6] and avoids any delay in the recognition and management of this unusual entity.
The presence of an appendix within the femoral canal can be explained by the presence of an abnormally low/large caecum which causes the appendix to have a pelvic location [4]. The CT findings in our patient show a very long appendix (10 cm) extending from an anatomically normal caecum with the tip extending through the femoral canal and explains another plausible mechanism for a de Garengeot's hernia. The aetiology of appendicitis has long been recognized as due to intraluminal obstruction either by a fecolith, worms, tumours or lymphoid hyrperplasia [7]. It is also possible that the rigid and narrow confines of the femoral canal can lead to extraluminal obstruction of the vermiform appendix and lead to ischaemia, inflammation, necrosis and subsequent perforation.
Management of a de Garengeot's hernia often involves repair of the femoral hernia and appendicectomy [3–5, 8]. Most authors agree that primary suture repair of the hernia is feasible, especially in the presence of an acutely inflamed or perforated appendix. However, the use of a mesh repair is a reasonable alternative when a normal appendix is found intra-operatively [9]. This is the first documented report of a de Garengeot's hernia managed with an open inguinal repair and laparoscopic appendicectomy and provides an alternative management for these rare hernias. Additionally, when recognized preoperatively, it allows the surgeon to consider a totally minimally invasive approach.



