-
PDF
- Split View
-
Views
-
Cite
Cite
Naji Abdallah Dabboussi, Riad Rifaat Fakih, Talal Adnan Kassar, Houssam Khodor Abtar, Occult closed posterior elbow dislocation with intimal rupture of the brachial artery in a 71-year-old male, Journal of Surgical Case Reports, Volume 2014, Issue 12, 1 December 2014, rju140, https://doi.org/10.1093/jscr/rju140
Close - Share Icon Share
Abstract
Posterior elbow dislocation with vascular injury is rarely encountered, but it is crucial for every emergency physician to diagnose it. Missing these injuries can result in neurovascular compromise, which in turn can lead to limb ischemia, compartment syndrome and potential limb loss. Having a normal X-ray on presentation makes this injury more difficult to diagnose. In this study, we present a case of occult posterior elbow dislocation with an intimal injury of the brachial artery. The rarity of these cases, the diagnostic modalities and the treatment options will be reviewed.
INTRODUCTION
Posterior elbow dislocation is the most common type of elbow dislocation with slightly higher incidence in the male population and they constitute ∼10–25% of all injuries to the elbow among persons with a mean age of 30 years [1].
The human instinct to protect the dominant arm from injury during fall is responsible for a slight predominance for dislocation in the nondominant extremity [2].
A high index of suspicion should be maintained by the emergency physician in evaluation for neurovascular compromise in all cases with elbow dislocation, especially in cases where the X-ray is normal.
In most of the times, a simple lateral view X-ray shows the dislocation, and absent radial and ulnar pulses insures that an arterial injury is present. In our case, the X-rays were normal, and the patient had normal pulses on presentation.
CASE REPORT
A 71-year-old right-handed male presented to our emergency department (ED) with left elbow pain after he fell on his left outstretched hand 1 h prior to presentation.
Physical examination revealed a swollen elbow, with a dusky cold hand; radial and ulnar pulses were initially felt and were weak in comparison with the contralateral side, but after repeated assessment, the pulses became absent.

Posterior splint was applied in ED and X-rays showed no fracture, no dislocation.
As arterial injury was suspected, angiography was done and revealed a brachial artery occlusion proximal to its bifurcation with the presence of some collateral circulation reaching and perfusing the radial and ulnar arteries.

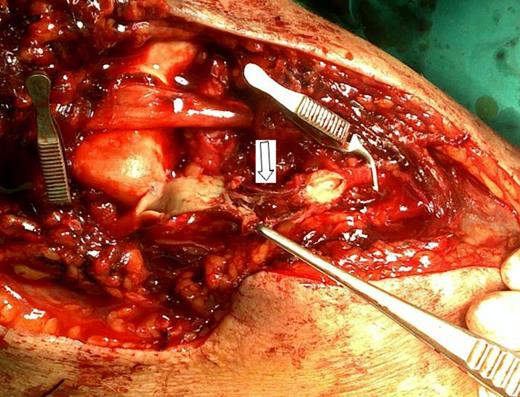
Intact adventitia of the brachial artery (arrow), also the median nerve seen stretched over the articular surface of the distal part of humerus, is intact (scissors).
Loss of intima in all the entire circumference of the brachial artery in a 1-cm segment (arrow).
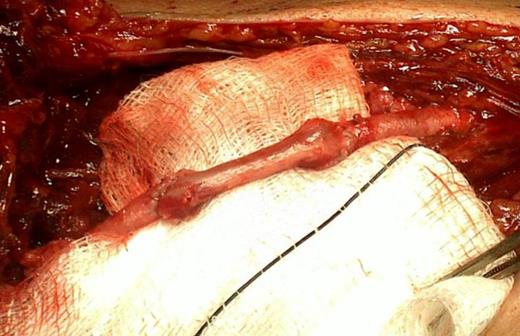
Complete arterial repair using an end-to-end reversed saphenous bridge.
Radial and ulnar pulses were regained directly postoperatively together with a normal color and warmth of the upper extremity, vascular observation was done to rule out compartment syndrome.
In the postoperative period, the elbow was immobilized for 3 weeks with a posterior splint in 70° flexion, then active range of motion exercises was started. At 1-year follow-up, patient regained all activities, and had nearly full range of motion, but with 15° loss of extension.
DISCUSSION
Elbow dislocation remains the third in occurrence after the shoulder and patellar dislocations [3]. The frequency of vascular involvement associated with closed elbow dislocation remains difficult to establish because the literature only reports short series of sporadic case studies, it approaches 4.3% [4], and in some series, as low as 0.47% reported by Spark et al. [5] who had 3 cases of vascular injury out of 634 closed elbow dislocation.
While reviewing the literature, we found only one case of brachial artery injury that was reported in the Middle East and was treated conservatively [6]. This leads us to the fact that these types of injuries are either missed because of collateral circulation or underreported due to the lack of research and proper documentations.
Whenever there is a suspicion of arterial damage, angiogram should be performed immediately and it still considered the gold standard for evaluation of arterial injury [7]. Sparks et al. [5] reported that only 12 of 30 cases of closed dislocation investigated for arterial insufficiency by angiography had arterial injuries.
Having a positive pulses do not rule out brachial artery injury as patient can have a well-developed collateral circulation around the elbow [8].
In our case, patient first had a weak pulse, then it became absent, and this could be explained by two theories. First, an intact collateral circulation perfusing the radial and ulnar arteries [9] and with ongoing elbow swelling, these collaterals were gradually compromised leading to impaired blood flow, and fading of the pulses [5]. Secondly, it can be explained by the fact that the initial injury caused only an intimal injury, that was not sufficient to cause a complete brachial artery occlusion, but an ongoing thrombosis formation on top of the intimal injury was occluding it gradually [8].
Although radiograph with lateral view of the elbow shows clearly a dislocation when present, most of the spontaneous reduction can be misleading and the injury will be overlooked. Only two cases of occult elbow dislocation with vascular injury were reported in the literature, and in both cases, there was a complete rupture of the brachial artery [8].
Few are the cases of intimal injury associated with elbow dislocation causing acute limb ischemia, in comparison with complete arterial transection; due to the rarity of the condition, few are the articles showing the prevalence of this type of arterial injury.
Concerning the management, it is now generally accepted that the standard of care is repair or reconstruction of a brachial artery injury [10].
To our knowledge, the combination of occult elbow dislocation with intimal injury of the brachial artery in a 71-year-old male makes this case to be the first reported in the literature.
In conclusion, palpable pulses after elbow dislocation should not rule out arterial injury and arteriogram should be done in case of suspicion of vascular injury as it is the gold standard of diagnosis in these injuries.
Finally, one should not be misled by ‘normal’ radiographs as they show only the position of the joint at the time the radiographs was taken, and not the time of injury. If the clinical picture is in out of proportion with the X-ray findings, the case should be dealt with caution, and further investigations should be done.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
Author notes
No previous communication to a society or meeting.



