-
PDF
- Split View
-
Views
-
Cite
Cite
Naohiro Nose, Tetsuya So, Atsushi Sekimura, Takeaki Miyata, Takashi Yoshimatsu, Yasuji Matsuno, The diagnosis of primary cardiac lymphoma was facilitated by computed tomographic coronary angiography, Journal of Surgical Case Reports, Volume 2014, Issue 12, 1 December 2014, rju137, https://doi.org/10.1093/jscr/rju137
Close - Share Icon Share
Abstract
Primary cardiac lymphoma (PCL) is a rare entity that leads to fatal symptoms such as serious arrhythmia. The present case was an 80-year-old female with severe dyspnea caused by 30 bpm bradycardia. Computed tomography revealed a tumor invading to the right inferior myocardium. A computed tomographic coronary angiography (CTCA) study revealed the right coronary artery penetrating the tumor with no invasion by the surrounding tumor. Because a percutaneous biopsy was unsuccessful, video-assisted thoracic surgery (VATS) was performed. The final pathological diagnosis was diffuse large B cell lymphoma. Rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP) chemotherapy reduced the size of the tumor, and the symptoms thereafter improved. An observation of the coronary artery penetrating the tumor without tumor invasion may be a characteristic finding of PCL. CTCA is useful to detect this finding. When a percutaneous biopsy is unavailable, VATS should be considered as a minimally invasive procedure to obtain a reliable diagnosis of PCL.
INTRODUCTION
Primary cardiac lymphoma (PCL) is a rare entity that comprises only 0.5% of extranodal lymphomas [1] and accounts for only 1.3% of cardiac tumors [2]. This tumor leads to fatal symptoms, such as congestive heart failure, pericardial effusion or arrhythmia [3]. Once a diagnosis of this tumor is made, chemotherapy can often improve the patient's prognosis [2]. However, the fact that there are few specific findings of this tumor and the poor condition of the patient often makes an antemortem diagnosis difficult [1, 2].
Computed tomographic coronary angiography (CTCA) is a relatively new, easy and non-invasive procedure that can be used to evaluate the condition of the coronary artery. We here report a case of PCL in which CTCA provided a clue to the diagnosis.
CASE REPORT
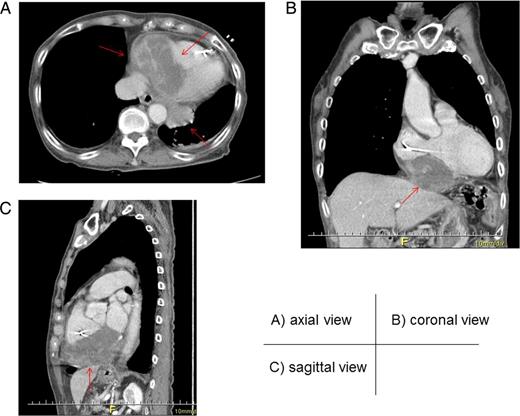
Axial (A), coronal (B) and sagittal (C) views of enhanced computed tomography. A tumor (arrow) measuring 90.0 × 56.4 × 60.0 mm, with heterogenous low enhancement and an unclear border invaded into the inferior myocardium.
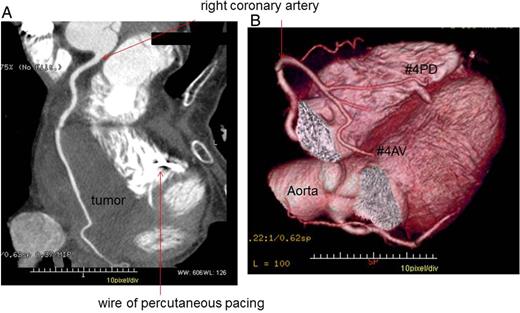
Computed tomographic coronary angiography. The right coronary artery penetrated the tumor with no significant signs of invasion (A) or displacement (B). The wire used for percutaneous pacing was placed in the right ventricle.
The perioperative pathological diagnosis ensured that a sufficient amount of malignant tumor had been harvested for a diagnosis. No complications developed during the perioperative period. The temporary pacing electrode was changed to a permanent pacemaker 5 days after the surgery. The final pathological diagnosis was diffuse large B cell lymphoma (DLBCL).
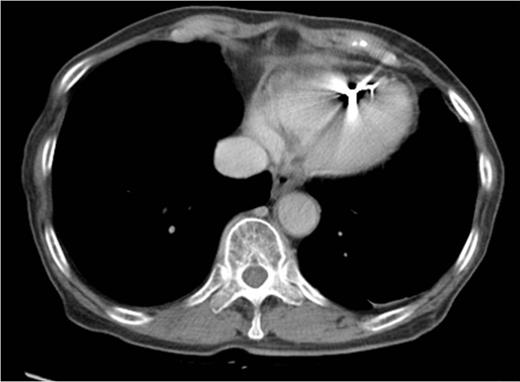
Enhanced computed tomography after chemotherapy. The tumor could not be detected.
Ten months after the surgery, local recurrence of the tumor was identified. The patient did not wish to receive any further treatment, and died 13 months after the surgery due to progressive disease.
DISCUSSION
PCL often leads to the development of severe arrhythmia, obstruction of blood flow, tumor emboli, treatment of refractory heart failure, dyspnea, superior vena cava syndrome and stroke [5]. These serious symptoms are attributable to the fact that over 90% of these tumors have pericardial involvement and are disseminated at the initial presentation [6]. These serious situations may lead physicians to avoid performing an aggressive pathological diagnosis by invasive procedures, either because it seems unfeasible or due to perceptions that it would not contribute to the subsequent treatment. Indeed, radiotherapy for PCL does not seem to improve the survival rate, and a radical surgical approach is not recommended [3].
However, PCL is classified mainly as DLBCL (60–80% of cases), and DLBCL has a good response to well-tolerated chemotherapy [2]. After eight cycles of R-CHOP every 3 weeks for Stage III or IV DLBCL, patients with a performance status of 0–2 showed a complete response rate of 76%, a 2-year survival rate of 70% and 80% of patients are able to undergo scheduled therapy [4]. Morita et al. [2] reported the use of rituximab monotherapy for an elderly hemodialysis patient with PCL, and indicated that it led to a good response and improvement of the symptoms without serious adverse effects. Unfortunately, the tumor in our case relapsed. However, the patient experienced an ∼10-month long disease-control period. When PCL is suspected, physician should consider making an active diagnosis, even if the patient's condition is poor, because good results may be obtained with chemotherapy.
No specific findings for PCL have been reported. Most of the tumors seem to appear as poor enhancement structures infiltrating adjacent chambers [7]. It often involves the right atrium and the conductive system, thus leading to many types of arrhythmias [8]. On the other hand, lymphoma tends not to invade large vessels because it is softer than the other malignant tumors [9]. Indeed, in our case, the right coronary artery penetrated the tumor without any signs of invasion, even though the tumor infiltrated the adjacent right chambers. This is the first case report that has described the CTCA findings of PCL. The observation of the coronary artery without invasion by the tumor may be a significant finding of PCL. Further accumulation of cases will be needed to determine whether such findings of CTCA are useful for the diagnosis of PCL.
To avoid thoracotomy, percutaneous tumor biopsy should be initially selected as a non-invasive method for making a pathological diagnosis [3]. When it is unavailable, biopsy via VATS should be selected as a less invasive procedure than thoracotomy. Our case went into shock due to severe bradycardia. Although the patient's condition had been very poor, we were still able to perform the tumor biopsy safely and easily via VATS with a temporary pacemaker. We believe that tumor biopsy via VATS is feasible whenever the patient's condition will allow general anesthesia to be tolerated.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- cardiac arrhythmia
- myocardium
- coronary angiography
- doxorubicin
- bradycardia
- coronary artery
- surgical procedures, minimally invasive
- computed tomography
- right coronary artery
- dyspnea
- biopsy
- chemotherapy regimen
- cyclophosphamide
- diffuse large b-cell lymphoma
- prednisolone
- thoracic surgery, video-assisted
- vincristine
- diagnosis
- neoplasms
- rituximab
- primary cardiac lymphoma
- tumor cell invasion
- r-chop



