-
PDF
- Split View
-
Views
-
Cite
Cite
Jens Heyn, Hanna Zimmermann, Alexander Klose, Benjamin Luchting, Christian Hinske, Mojtaba Sadeghi-Azandaryani, Idiopathic internal mammary artery aneurysm, Journal of Surgical Case Reports, Volume 2014, Issue 12, 1 December 2014, rju125, https://doi.org/10.1093/jscr/rju125
Close - Share Icon Share
Abstract
Aneurysms of the internal mammary artery are extremely rare, and their presentation and treatment are variable. Since these aneurysms often tend to rupture and cause haemothorax and life-threatening conditions, the knowledge of secure treatment options is indispensable. We here report the case of an idiopathic internal mammary aneurysm in a 46-year-old man. Open surgical resection of the aneurysm was performed in this case without any complications. The postoperative course was uneventful and the patient was in a good physical condition without any vascular or neurological abnormalities during follow-up.
INTRODUCTION
Aneurysms of the internal mammary artery (IMAA) are uncommon clinical entities [1] and usually occur in patients after sternotomy, placement of a central venous catheter or pacemaker leads [2]. Less common, these aneurysms are associated with vasculitis (e.g. Kawasaki disease [3]), connective tissue disorders (e.g. Marfan syndrome [4]), chest wall infections [5] or atherosclerosis [6]. However, changes in the structure of the vascular wall at the cellular level such as cystic medial necrosis or hyperplasia lead to loss of elasticity and formation of aneurysms [6].
Since rupture of IMAA leads to haemothorax and life-threatening conditions, early diagnosis and treatment is indispensable. We here report the case of a 46-year-old man with an idiopathic IMAA.
CASE REPORT

Phlebography reveals a compression of the left subclavian vein.
Due to the symptoms and the suspicion of malignant tumour, an open resection was intended. Therefore, the patient was placed in a lateral position with the right arm freely moveable. Transverse incision was made below the axillary hairline between the pectoralis major and latissimus dorsi muscle, followed by careful preparation of the first rib, layer by layer. Resection of the first rib was done among sternocostal and costovertebral joint after accurate separation from the underlying pleura. Medial of the pleural cupula a boorish tumour was palpable and the left IMA was walled by this tumour. Therefore, the tumour and the left mammary artery were removed after cautious preparation. After careful arrest of bleeding, the wound was stepwise closed with single button sutures.

MRI scan of the thorax shows a tumour at the left pleural cupula.
DISCUSSION
The IMA arises from the first portion of the subclavian artery and immediately passes downwards close to the pleura within the upper intercostal space. Further distal, it proceeds anteriorly to the transversus thoracic muscle to end in the sixth intercostal space by dividing into the superior epigastric and musculophrenic artery [7]. This anatomical course makes the IMA vulnerable to severe deceleration or penetrating injuries [7].
Infections or genetic disorders are also frequent causes of IMAAs [3–5, 8]. A spontaneous development of an IMAA without a rememberable trauma or injury as described in our case is a rarity. Due to the low prevalence of IMAAs, informations regarding diagnosis and secure treatment options are scarce [1]. IMAAs typically appear with haemoptysis, cough and dyspnoea. In some patients, IMAAs only emerge as a bulging chest mass [8].
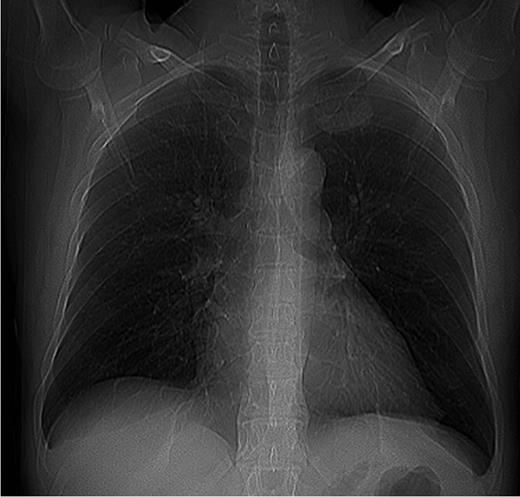
However, chest X-ray should be performed as first step when IMAA is suspected. An additional CT scan conceivably in combination with an angiography is a valuable method to localize the IMAA and to plan the surgical procedure [1]. In our patient, classical symptoms of an IMAA were missing and the IMAA was an incidental finding within routine X-ray. The compression symptoms of the IMAA were only found after accurate request and examination. The additional imaging procedures failed to confirm the diagnosis.
Prior to therapy, treatment options should be carefully considered. Open surgical repair, stent implantation or coil embolization has been described in the literature [1, 9, 10]. Even though long-term results are missing, coil embolization or stent implantation has become the treatment option of choice in minor aneurysms due to the minor invasivity of these procedures [3, 10]. Despite this advantage, we were not convinced with coil embolization or stent implantation because of the following reasons:
A malignant process could not be excluded by the imaging prior to surgery.
Even if the diagnosis of an IMAA would have been made, the compression of the adjacent vessels and nerves (which caused symptoms) would not have been treated by an endovascular procedure.
An idiopathic IMAA is an extremely rare entity. The diagnosis may be difficult, when clinical symptoms are missing. When the diagnosis of IMAA is made, prompt therapy is essential in avoidance of life-threatening events. Selection of the ideal approach depends on the underlying pathogenesis. Open surgical resection represents an invasive procedure with the option of decompressions of neighbouring structures, good postoperative outcome and without complications in our case.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
FUNDING
The author(s) received no financial support for the authorship, and/or publication of this article.



