-
PDF
- Split View
-
Views
-
Cite
Cite
Uchechukwu Stanley Ogu, Garrett Keim, Andrew J. Cleary, Robert S. Bloch, Atraumatic splenic rupture secondary to metastatic non-small-cell lung cancer, Journal of Surgical Case Reports, Volume 2013, Issue 7, July 2013, rjt051, https://doi.org/10.1093/jscr/rjt051
Close - Share Icon Share
Abstract
Splenic metastasis of solid organ tumors is rare; even more so is splenic rupture from metastatic disease. We report a case of a 61-year-old male who presented with splenic rupture and hemodynamic instability, secondary to malignant metastasis from a recently diagnosed left lung cancer.
INTRODUCTION
Splenic metastasis of lung tumors is rare. In a recent study, splenic metastatic disease from primary lung cancer was found in 15 of 267 autopsies [1]. This presentation was most common with advanced metastatic disease. One current hypothesis explaining the rarity of splenic metastasis in lung cancer is the filtration function of the spleen. The spleen, being the source of many pro-apoptotic factors that help to destroy aged granulocytes, may also help to destroy cancer cells that pass through the spleen. This case presents a patient with non-traumatic splenic rupture as the initial presentation of lung cancer metastasis.
CASE REPORT
A 61-year-old male presented with a 2-week history of worsening posterior neck and bilateral shoulder pain, and a several hour history of severe, left-sided abdominal tenderness. The patient reported no recent history of trauma. The patient had been diagnosed with poorly differentiated, left lung adenocarcinoma 5 months prior; he was status-post left upper lobectomy. PET scan, at that time (Fig. 1), showed no evidence of metastatic disease and the pathologic staging was determined to be T2aN0M0 (Stage 1B).
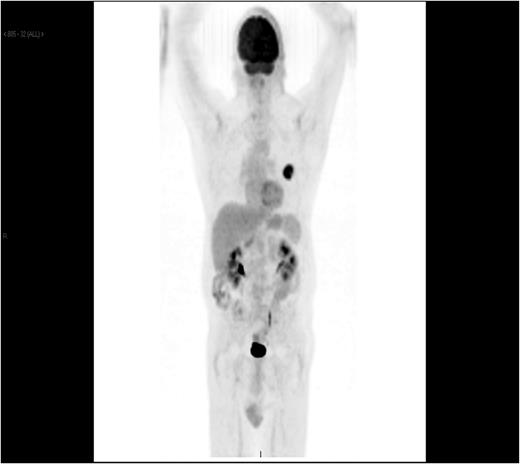
PET CT showing left lingular malignancy and no evidence of metastasis.
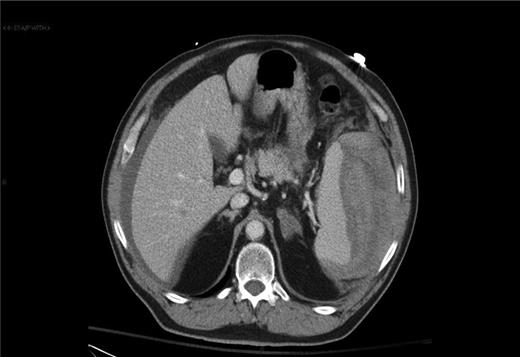
In the emergency department on current presentation, the patient was hypotensive with a blood pressure of 76/40. Physical examination revealed a soft, distended abdomen that was tender in the left upper quadrant. The patient demonstrated no rebound tenderness or guarding. CT scan of the chest, abdomen and pelvis revealed hemoperitoneum and a possible splenic laceration (Fig. 2). Laboratory work showed hemoglobin of 10.9 g/dl and a hematocrit of 30.4%. The patient was optimized for emergent exploratory laparotomy.
Surgery revealed gross, metastatic lesions in the spleen and mesentery. A splenectomy with en bloc resection of the involved mesentery was preformed. The resected specimens all revealed metastatic, poorly differentiated non-small-cell carcinoma; consistent on immunoperoxide staining with the previously known primary lung cancer diagnosed and treated 4 months prior.
Further workup on this patient revealed a final diagnosis of stage IV non-small-cell lung cancer with metastases to the liver, mesentery, spleen and cervical spine. The patient was started on radiation therapy, but eventually refused more treatment due to the pain he was experiencing. The patient died <1 month later.
DISCUSSION
The initial presentation of lung cancer metastasis as a splenic rupture is a very rare event. Review of literature shows only seven cases of spontaneous splenic rupture due to metastatic lung cancer [2, 3]. This appears to be the first case in literature in which disseminated metastatic adenocarcinoma of the lung presented with spontaneous splenic rupture. Previous cases of splenic rupture were seen as an occult presentation of lung cancer [3] and as a solitary metastatic lesion [4].
Autopsy studies have shown splenic metastases to be present in 2.3–7.1% of patients with cancer. Autopsy studies have also shown melanoma of the skin to be the most common cancer to metastasize to the spleen [5]. A 25-year uni-institutional study of splenic metastasis showed that only 7 of 92 patients with splenic metastasis were symptomatic. Of these seven, only two cases involved a rupture of the spleen, yielding a splenic rupture rate due to metastasis of only 2.17% [6]. This same study showed that the splenic metastases where found 15 months to 2 years after the discovery of the primary tumor [6].
The patient in this case presented with splenic rupture only 5 months after the initial diagnosis of lung cancer and 4 months after surgical resection. Staging workup at the time showed no metastatic lesions.
In conclusion, splenic metastasis of lung cancer is a rare phenomenon, which is usually asymptomatic. In patients with history of lung cancer presenting with splenic rupture and no history of trauma, the possibility of metastasis to the spleen should be an included differential diagnosis.



