-
PDF
- Split View
-
Views
-
Cite
Cite
Noel P. Lynch, Mark A. Corrigan, David E. Kearney, Emmet J. Andrews, Successful laparoscopic management of an incarcerated obturator hernia, Journal of Surgical Case Reports, Volume 2013, Issue 7, July 2013, rjt050, https://doi.org/10.1093/jscr/rjt050
Close - Share Icon Share
Abstract
Obturator hernia is a rare pelvic hernia that occurs primarily in multiparous, elderly (>70 years of age), thin females. This case highlights the successful laparoscopic mesh repair of an incarcerated obturator hernia in an octogenarian.
The authors report a case of an incarcerated obturator hernia in an elderly female with subsequent high-grade small bowel and its successful laparoscopic operative management. A review of the relevant literature was also performed following a search on the online literature databases such as PUBMED and EMBASE. Laparoscopic mesh repair of the incarcerated obturator hernia and an ipsilateral femoral hernia found incidentally was successfully performed. A review of the literature showed a significant burden of morbidity and mortality associated with obturator hernias. Laparoscopic mesh repair has been previously shown to be a safe therapeutic modality. Small bowel obstruction and leg pain in a thin elderly lady should arouse suspicion for an incarcerated obturator hernia. Laparoscopic management of an incarcerated obturator hernia is a feasible and safe therapeutic option.
INTRODUCTION
Obturator hernia is a rare finding on acute surgical wards. It accounts for <1% of all hernias [1]. Typically, they manifest in multiparous, thin females within their seventh to ninth decades of life [2]. Patients frequently present with symptoms of intestinal obstruction and, occasionally, pain along the distribution of the obturator nerve on the ipsilateral side (Howship–Romberg sign) [3]. However, the diagnosis can be difficult to make and delay in diagnosis and surgical intervention contributes directly to high morbidity and mortality rates [4]. The authors report the successful laparoscopic management of an acute presentation of an obstructed obturator hernia.
CASE REPORT
An 85-year-old female with a background of trans-abdominal hysterectomy, hypertension and a previous thyroid lobectomy, presented acutely with a 1-day history of upper abdominal pain radiating down her left leg associated with numerous episodes of emesis. Her bowels had opened three times in the previous 24 h. She was anorexic for the previous 24 h. She reported a similar episode requiring hospitalization 3 weeks before, which was treated non-operatively in another institution.
On examination, her vitals were stable. She displayed mild upper abdominal tenderness without signs of peritonism. Bowel sounds were present. Her haematological investigations were unremarkable. A plain film of abdomen was unremarkable. She was treated presumptively as a small bowel obstruction and non-operative measures were employed and the patient proceeded to have a computed tomography (CT) scan of the abdomen and pelvis, which indicated proximal small bowel obstruction secondary to a left obturator hernia (Fig. 1). She proceeded to emergent laparoscopy and subsequent mesh repair of left obturator hernia, containing an obstructed loop of small bowel. There was a concomitant femoral hernia that was repaired separately.

CT image. Proximal small bowel obstruction secondary to a left obturator hernia within white outline.
Under general anaesthetic, the optical technique for access was utilized at the umbilicus with a 5 mm port. Two further working ports, a 5 and 10 mm, were placed in the right lower quadrant and right hypochondrium, under direct vision. Findings included visualization of small bowel dilatation down to small bowel in a left obturator hernia with an incidental left femoral hernia containing omentum (Fig. 2). The incarcerated small bowel was reduced using a pair of non-traumatic forceps and deemed viable. The omentum was reduced from the femoral hernia.
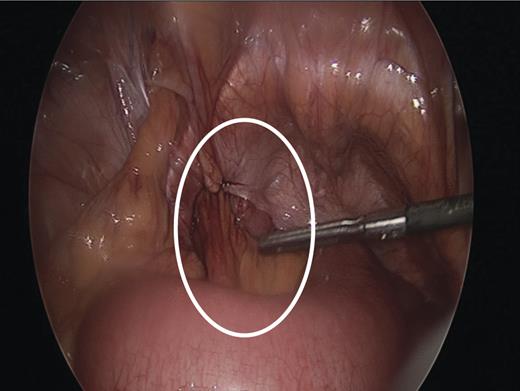
Intraoperative image showing left sided obturator hernia within white outline and incidental femoral hernia at 11’o clock position.
The obturator hernia was repaired with Proceed™ Ventral patch (Ethicon, Inc., Sommerville, NJ, USA) tacked with AbsorbaTack™ (Covidien, Mansfield, Inc., MA, USA) fixation device. The initial fixation was performed onto Cooper's ligament. This then allowed the mesh to be spread laterally and fixed to the transversalis fascia. The femoral hernia was repaired with 2 × 2/0 Vicryl (Ethicon, Inc., Sommerville, NJ, USA) sutures placed laparoscopically. Port sites were closed in a routine manner. The patient did suffer a post-operative pneumonia but was treated appropriately, made a good recovery and was discharged home well.
DISCUSSION
Obturator hernia was first described in 1724 by Amaud de Ronsil [3]. Conditions associated with long-standing increased intra-abdominal pressure, weight loss that leads to a decreased peritoneal fat and multiparity are implicated on the basis of laxity of the parietal peritoneum [4]. All are believed to increase the risk for development of an obturator hernia and women are affected nine times more frequently than men [1].
The obturator foramen is formed by the continuity of the pubic and ischial rami. The obturator membrane covers most of the foramen, except at the anterior superior aspect. The obturator vein, artery and nerve branches traverse its superior angle. It is also through this defect that the hernia descends. The anatomic formation of obturator hernia has been previously described in detail in the literature [4], but the basic premise of the aetiology and pathogenesis is based on the loss of preperitoneal fat or lymphatic tissue that occupies the obturator canal [5].
Clinical symptoms vary and are non-specific. Previous authors have proposed four ‘classic’ features of an obturator hernia: (i) a palpable mass in the groin with the patient supine, and the thigh flexed, adducted and rotated laterally; (ii) intestinal obstruction; (iii) previous attacks of bowel obstruction resolving spontaneously; (iv) the Howship–Romberg sign. The Howship–Romberg sign is medial thigh and hip pain exacerbated by adduction and medial rotation of the thigh and relieved by thigh flexion. It is reportedly present in 15–50% of obturator hernia patients [6].
The usefulness of CT in diagnosis was first reported by Cubillo in 1983 and it has been assisting in the earlier diagnosis of obturator hernia but despite this post-operative mortality has not improved remarkably [7].
The management of an obturator hernia is surgery. Traditionally laparotomy has been the most common surgical approach [8]. However, several studies have shown the feasibility of laparoscopic techniques for the management of incarcerated obturator hernia [9]. The transabdominal preperitoneal repair for obturator hernias is the preferred technique as it allows assessment of the visceral contents.
Various procedures for closure of the hernia defect have been advocated. These include simple peritoneal closure, local flaps using periosteum or uterine ligament. The current trend is to repair the defect using prosthetic material; however, there is no robust evidence in the literature to compare and contrast the superiority of mesh repair over other repairs in obturator hernia [10].
In conclusion, we present this rare case to raise awareness of a rare presentation but with significant morbidity and mortality if a high index of suspicion is not maintained. This case illustrates the usefulness of CT in diagnosing obturator hernia and it also confirms that laparoscopic mesh repair of an incarcerated obturator hernia is safe and technically feasible.



