-
PDF
- Split View
-
Views
-
Cite
Cite
Simon A. Fallis, Lewis H. Taylor, R.M.R. Tiramularaju, Biological mesh repair of a strangulated perineal hernia following abdominoperineal resection, Journal of Surgical Case Reports, Volume 2013, Issue 4, April 2013, rjt023, https://doi.org/10.1093/jscr/rjt023
Close - Share Icon Share
Abstract
Perineal hernia is a recognized but uncommon complication following proctectomy. Emergency presentations of this hernia are very rare and are not well described in the literature. We present the case of an 81-year-old lady who presented with small bowel obstruction with strangulation secondary to a perineal hernia 2 years after abdominoperineal resection for carcinoma of the rectum. At laparotomy, a small bowel resection was required and a biological mesh was used to repair the perineal defect.
INTRODUCTION
Perineal hernia is an uncommon but recognized complication of abdominoperineal resection of the rectum. Emergency presentations of post-operative perineal hernia are very rare and not well described in the literature. We present a case of small bowel obstruction with strangulation secondary to a perineal hernia and the surgical technique employed to repair the defect.
CASE REPORT
An 81-year-old lady presented to the on call general surgeons with abdominal pain and vomiting for 24 hr. Two years previously she had undergone a laparoscopic abdominoperineal resection for carcinoma of the rectum at another centre. She had not previously received radiotherapy and was a non-smoker. History, examination and abdominal X-ray suggested small bowel obstruction. On admission, there were no signs of peritonism, observations were normal and markers of inflammation were not significantly raised.
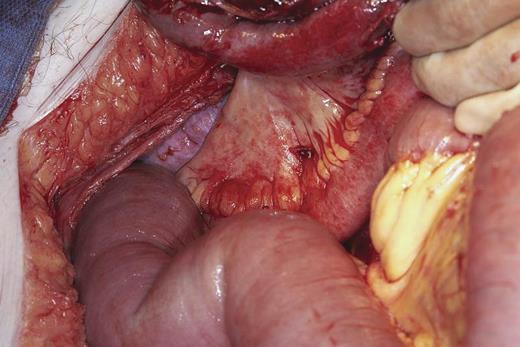
Although not known to have a hernia, she described discomfort and swelling in her perineum over the previous year that sometimes made it difficult to sit down. Direct examination of the perineum confirmed the presence of an irreducible but non-tender hernia (Fig. 1). Conservative treatment with nasogastric drainage and intravenous fluids produced no clinical improvement. The following morning a CT of the abdomen and pelvis was performed which confirmed small bowel obstruction and revealed a cut off at the neck of a perineal hernia.

Clinical examination of the perineum revealing perineal hernia.
At operation, small bowel obstruction was found with volvulus of a loop of ileum around an adhesion at the neck of the perineal hernia (Fig. 2). Around 80 cm of gangrenous mid-ileum was resected and a primary end-to-end anastamosis performed. After thorough washout of the abdomen and pelvis, the wide pelvic floor defect was bridged with Strattice™ Tissue Matrix, secured in place with 2.0 prolene sutures (Fig. 3). An omental pedicle graft was used to cover the mesh and fill the pelvis. One abdominal tube drain and two perineal suction drains were inserted and removed over the course of the next 7 days.
Laparotomy findings of transition point of small bowel obstruction at neck of perineal hernia.
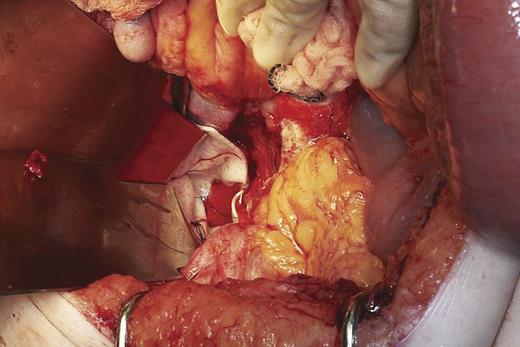
Bridging of perineal defect with Strattice™ Tissue Matrix before covering with omentum.
The patient made an uncomplicated recovery and was discharged home. At 6 months follow-up, she remained well with no reported problems other than a slight increase in stoma activity. There was resolution of her previous perineal symptoms and no clinical recurrence of the hernia.
DISCUSSION
Perineal hernia is an uncommon but well-documented complication of abdominoperineal resection of the rectum. The reported incidence is between 0.34% [1] and 7% [2], but there may be significant under reporting by patients who experience minimal symptoms or do not report them to their surgeon. A hernia may become evident up to 5 years following surgery [3] and risk factors for development include neo-adjuvant chemo-radiotherapy and smoking. When recognized, many are treated conservatively but repair is indicated for symptoms such as pain, skin erosion and intermittent obstruction.
Surgical repair can be a challenge, and trans-abdominal, perineal and combined approaches have been described [3]. More recently laparoscopic approaches have been advocated [4]. Reconstruction of the pelvic floor defect has been described with various types of synthetic and biological mesh as well as myocutaneous grafts such as a vertical rectus abdominis flap [5].
Emergency presentations of post-operative perineal hernia are very rare. Relief of obstruction and bowel resection are best performed through a midline laparotomy. Synthetic meshes are contraindicated in the presence of contamination from non-viable bowel or bowel contents. Reconstruction using myocutaneous flaps is a specialist, time consuming procedure with an appreciable morbidity and usually inappropriate in an acute setting.
The use of a biological mesh, or acellular porcine dermal matrix, has the advantage of a low risk of infection when used in a potentially contaminated field. Combined with an omental pedicle graft to fill the pelvic space, this produced a safe and effective repair. This has not been previously described in the emergency setting for a strangulated perineal hernia.
In the era of extra-levator abdominoperineal resection, prophylactic repair of the perineal defect has become a standard for many. It remains to be seen whether this practice will lead to a change in the reported incidence of perineal hernia.
Although rare, strangulation of a post-operative perineal hernia can occur and should be considered when assessing patients with a history of proctectomy and small bowel obstruction. Examination of the perineum should always be performed. Where repair of a perineal defect in potentially contaminated circumstances is anticipated, an appropriate biological mesh can be selected and careful preoperative planning is required.



