-
PDF
- Split View
-
Views
-
Cite
Cite
Oladejo Olaleye, Shizalia Salleh, Don David, Richard Bickerton, Lacrimal sac compression by an anterior ethmoidal mucocele presenting as a late complication of dacryocystorhinostomy, Journal of Surgical Case Reports, Volume 2013, Issue 2, February 2013, rjt002, https://doi.org/10.1093/jscr/rjt002
Close - Share Icon Share
Abstract
This was an unusual case of lacrimal sac compression by an anterior ethmoidal mucocele presenting as a late complication of a dacryocystorhinostomy (DCR) that was jointly managed by ophthalmic and ENT surgeons via an endoscopic approach. A 22-year-old lady presented with a 12-month history of a painless lump in her left medial canthus area and a 6-month history of left intermittent epiphora. She had a DCR when she was 15 years old with initial symptom control until recent recurrence. There were no nasal or other eye symptoms. The rest of the eye and nasendoscopic examinations were unremarkable. An MRI scan suggested a dacryocystocele; however, a further CT scan revealed a 1.6 cm cystic lesion consistent with an anterior ethmoidal mucocele compressing the lacrimal sac. An endoscopic left anterior ethmoidectomy with marsupialisation of the mucocele was performed in combination with an endoscopic DCR. She made good post-operative recovery.
INTRODUCTION
Lacrimal sac compression from an anterior ethmoidal mucocele is unusual, especially as a late complication of dacryocystorhinostomy (DCR). We present the joint management of such a case by ophthalmic and ENT surgeons, describing the diagnostic dilemma and the intra-operative endoscopic techniques used.
CASE REPORT
A 22-year-old lady presented to the Joint Ophthalmology & ENT watery eye clinic with a 12-month history of a painless lump in the medial corner of her left eye, which was not increasing in size. Six months after noticing this painless lump, she developed left-sided intermittent epiphora. At the age of 10, she first had a watery left eye, and following a DCR when she was 15 years old, her symptoms seemed to resolve until this episode. She denied any nasal symptoms.
She had a history of depression, for which she was on fluoxetine but was otherwise well. She smoked three cigarettes per day and drank alcohol occasionally.
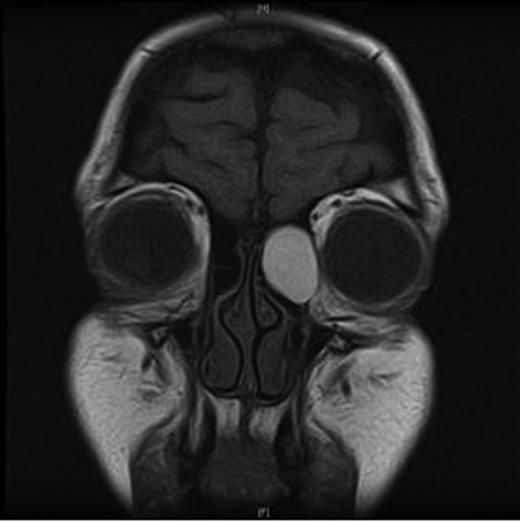
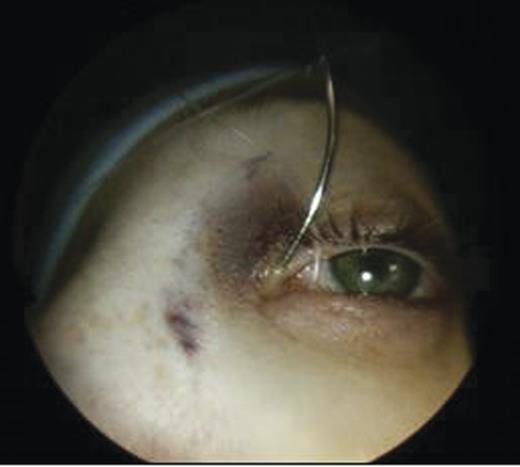
Clinical examination revealed a small cystic swelling in her left medial canthus (Fig. 1). There was no discharge on pressure, mild tenderness was elicited and the swelling was not compressible. The rest of the eye examination was normal with a visual acuity of 6/6 in both eyes.
Anterior rhinoscopy showed a reasonable nasal airway with healthy mucosal lining. Flexible nasendoscopy revealed no nasal lesions with the septum slightly deviated to the right.
An MRI scan of the orbits showed a well-defined, thin-walled 22 × 16 mm cyst medial to the left orbit containing fatty/proteinaceous material, which was lying within and mildly expanding the left ethmoid air cells (Figs 1–3).
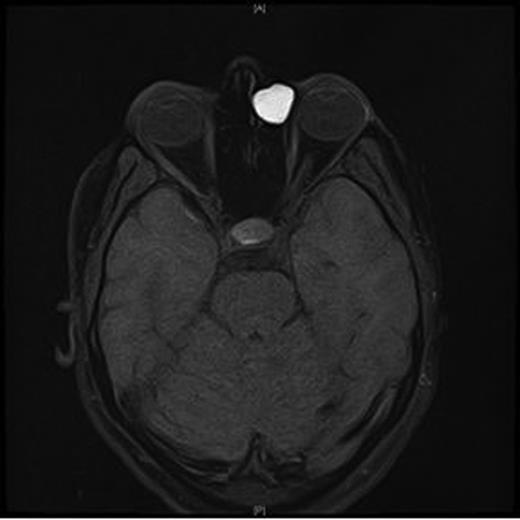
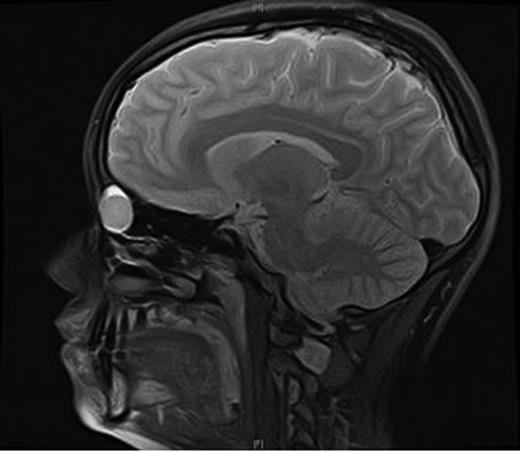
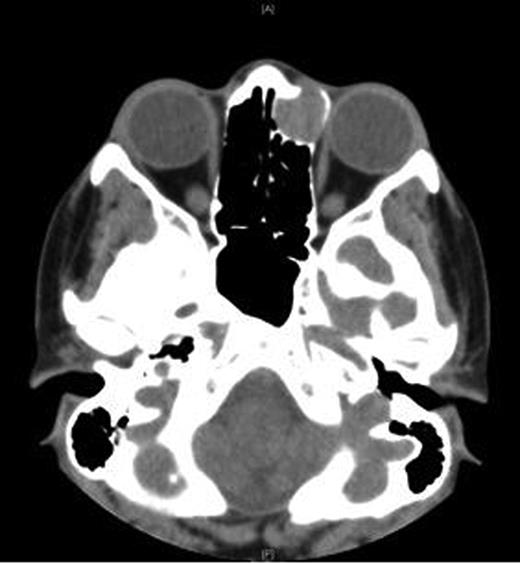
A CT scan of the paranasal sinuses and orbits revealed the cystic expansile 1.6 cm mass at the left medial canthus to be of soft tissue density. The lateral wall of the mass expanded outwards into the orbit (suggesting an anterior ethmoidal mucocele) rather than being pushed medially (which could have been indicative of a dacryocystocele) (Fig. 4).
All pre-operative blood tests were normal. A joint operating session by the ENT and Ophthalmic surgeons was planned with a view to performing an endoscopic left anterior ethmoidectomy with marsupialisation of the mucocele in combination with an endoscopic DCR.
Ophthalmic techniques
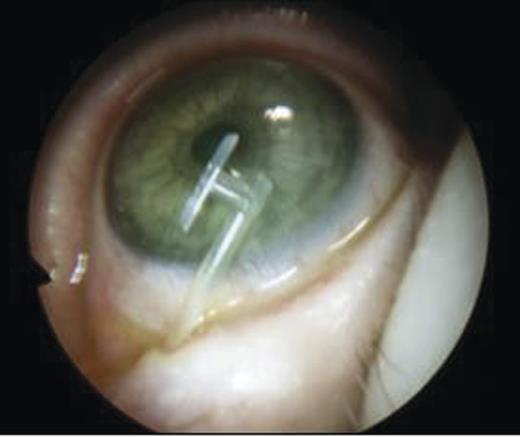
The puncti were probed (Fig. 5) and fluorescein dye instilled with no dye outflow to the left inferior meatus. It was not possible to pass the probe through the upper punctum so a mini-monoka DCR stent was inserted and secured (Figs. 6 and 7). Chloramphenicol eye drops were instilled.

Endoscopic Sinus Surgery techniques
The nasal cavity was prepared with modified Moffet's solution and a Storz 30° endoscope used with visualisation of the nasal cavity on a monitor.
- An inferiorly based mucosal flap was elevated on the lateral nasal wall (Fig. 8) with the incision performed using a small myotome.
Removal of part of the lateral nasal wall anterior to uncinate process was performed for access to the lacrimal system (unciformian endonasal DCR)
30° punch forceps were used to nibble bone sequentially for adequate exposure.
Further drilling of the lateral bony wall was undertaken with a small cutting burr.
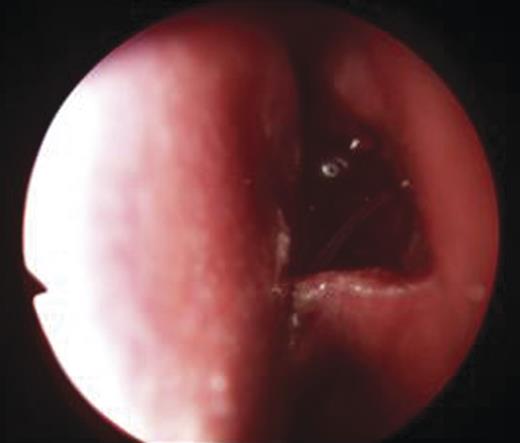
- An endoscopic left anterior ethmoidectomy was performed (Fig. 9) with marsupialisation of the mucocele (Fig. 9) and trimming of the DCR stent (Fig. 10)
 Figure 9:
Figure 9:Transnasal endoscopic left anterior ethmoidectomy and marsupialization of mucocele.
 Figure 10:
Figure 10:Post-operative view with trimmed DCR stent in situ in the left nasal cavity.
Post-operatively, she was discharged the next day and advised to administer chloramphenicol eyedrops as well as betnesol nasal drops for a week. The DCR stent remained in situ for 3 months and was removed in the clinic. There was clinical resolution of the medial canthal swelling and epiphora.
DISCUSSION
A mucocele is a benign, mucus-filled lesion lined by ciliated columnar epithelium. It gradually expands and may lead to bony erosion and remodelling. In the paranasal sinuses, it can occur primarily as a mucus retention cyst [1] or can be secondarily caused by obstruction of the sinus ostia due to infection, allergy, trauma or surgery. A secondary infection can cause a period of rapid expansion with complications [2].
Paranasal sinus mucocele is a relatively uncommon condition occurring most frequently in the frontal sinus followed by the ethmoid, sphenoid and maxillary sinuses. Sixty percent of mucoceles occur in the fronto-ethmoidal region and an isolated ethmoid mucocele is rare.
The clinical presentation depends on the site, size and extent of the mucocele. Patients usually present with eye symptoms rather than nasal or sinus symptoms [3]. These symptoms include headaches mainly in the periorbital region, exophthalmus, ophthalmoplegia, proptosis and diplopia. Posterior ethmoid and sphenoidal mucoceles can cause pressure on the optic nerve leading to visual loss. Other rare presentations have been reported, including a posterior ethmoid mucocele causing ipsilateral oculomotor nerve palsy [4] and an ethmoid mucocele causing acute severe orbital pain with non-axial proptosis without diplopia [5]. There is documented evidence that previous endoscopic sinus surgery can lead to paranasal sinus mucocele formation due to adhesion formation in the middle meatus causing obstruction to the sinus ostium. The development is usually delayed and may form several years after the original surgery [6]. An ethmoidal mucocele has also been reported after transpalpebral bony orbital decompression.
Known complications of DCR include adhesions [7], canalicular tear, sump syndrome, pyogenic granulomata and recurrence of epiphora. There are, however, no reported cases in English literature on the development of an anterior ethmoid mucocele as a delayed complication of a DCR causing lacrimal sac compression. To our knowledge, this case is the first to highlight such a correlation.
Joint management by Ophthalmic and ENT surgeons has been shown to yield good results. Paranasal sinus mucoceles can be effectively managed using the transnasal endoscopic approach and marsupialisation with complete recovery reported in 82–96% of cases, while an extranasal approach can be used for recurrence [8].
The unciformian endonasal DCR has been shown to have better outcomes [9]. There are currently newer techniques, including the translacrimal transnasal laser-assisted DCR using neodymium: YAG [10]. Mitomycin C has also been used to attempt to reduce adhesions but its efficacy is inconclusive.



