-
PDF
- Split View
-
Views
-
Cite
Cite
AM Felstead, PM Patel, PJ Revington, Submandibular gland mucocele presenting as a lateral neck swelling, Journal of Surgical Case Reports, Volume 2012, Issue 6, June 2012, Page 8, https://doi.org/10.1093/jscr/2012.6.8
Close - Share Icon Share
Abstract
Mucus extravasation cysts or mucoceles are an extremely rare occurrence in the major salivary glands. We report upon an unusual case of a submandibular gland mucocele presenting as a neck lump. It should therefore be considered in the differential diagnosis of swellings in the lateral neck. Diagnosis and management are complicated by their similarity to the plunging or cervical ranula and differentiation may be potentially difficult. Detailed imaging often reveals the plunging ranula as being characterised by a so –called ‘tail’ sign. In our case this sign was absent and subsequent excision confirmed origin from the submandibular gland. We discuss potential treatment modalities and propose a rationale for definitive management.
INTRODUCTION
Mucus extravasation cysts or mucoceles are an extremely common lesion of the minor salivary glands. It is however a rare occurrence in the major salivary glands (1). We report upon an unusual case of a submandibular gland mucocele presenting as a lateral neck swelling. The term plunging or cervical ranula refers to mucoceles that extend below the mylohyoid muscle, beyond the sublingual space and invariably are associated with the sublingual salivary gland. Differentiation from submandibular gland mucoceles is potentially difficult, though plunging ranula is usually characterised by a so –called ‘tail’ sign on imaging. In our case this sign was absent and subsequent excision confirmed origin from the submandibular gland. Submandibular gland mucocele should be considered in the differential diagnosis of lateral neck swellings.
CASE REPORT
A 54 year old woman presented with a large asymptomatic swelling of the right lateral neck. The swelling had been present for three months but had attained large dimension and was still felt to be increasing in size. She denied any history of trauma, surgery, infection, dysphagia, voice change or weight loss. She was a non-smoker.
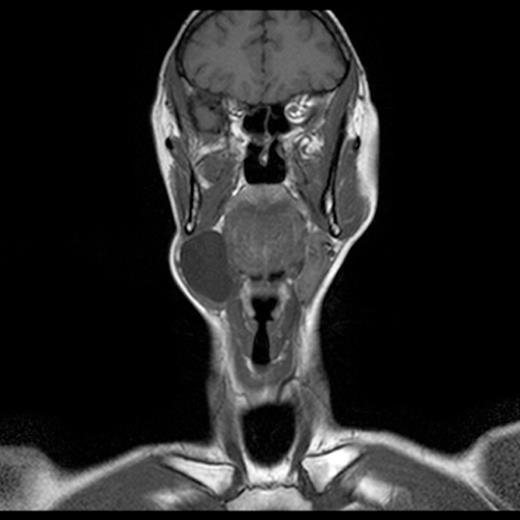
Examination of the oral cavity and oropharynx was unremarkable. Palpation of the neck mass revealed a soft, fluctuant, non-tender swelling approximately 6cm in diameter arising superficially within the right submandibular region. There was no associated cervical lymphadenopathy. A magnetic resonance imaging (MRI) scan revealed a large cystic structure in the right lateral neck involving the submandibular space (Fig 1). There was no ‘tail’ sign. No other abnormalities were demonstrated. Fine needle aspiration biopsy revealed abundant cystic fluid. The sample proved inadequate for cytological assessment, however was found to have a raised amylase and protein content suggesting salivary origin. Routine blood tests were all normal.
Under general anaesthesia the cystic mass was meticulously excised intact via a low submandibular incision. It was found to be in continuity with the ipsilateral submandibular gland (Fig 2). Histolopathology of the specimen confirmed a fibrous-walled retention cyst associated with a submandibular gland showing chronic obstructive changes. The patient made an uneventful post-operative recovery with no evidence of recurrence at six months.

Intraoperative photograph of the excised submandibular gland mucocele
DISCUSSION
The presentation of a submandibular gland mucocele is uncommon with only a few reported cases in the literature (1-3). It has been postulated that this rarity might be due to the anatomical location of the gland and the protective nature of the mandible1. Furthermore the physiology of the gland is such that unlike the sublingual gland, which exhibits continuous secretion, the submandibular gland secretes saliva only following stimulation (4). Nevertheless, despite the true aetiology being unknown it is thought likely that trauma, obstruction and congenital anomalies are most likely causes (5). The differential diagnosis of a submandibular gland mucocele should include the numerous inflammatory, infective, developmental and neoplastic processes affecting the lateral neck. In particular, a solitary cystic mass should be thoroughly investigated to exclude the possibility of cystic degeneration of a lymph node secondary to metastatic squamous cell carcinoma. Fine needle aspiration biopsy for cytological and biochemical assessment can confirm the nature of the cyst and is usually found to have a high amylase and protein content (6).
The management of a submandibular gland mucocele is potentially controversial and includes a number of treatment modalities that have been advocated in the management of the cervical or plunging ranula. Injection of scelorosing agents have been used to induce inflammation and fibrosis from within the lumen of the cyst thus sealing further extravasation. Aspiration is a simple technique but yields a high recurrence rate and as such its use has been largely restricted to the conservative management in the paediatric population. Marsupialisation has gained popularity not least because of its relative simplicity, but also because it involves only limited dissection and therefore a reduced risk of damage to adjacent structures. Recurrence however is unpredictable leading some authors to advocate a modified technique incorporating packing the cyst cavity (2). Contemporary opinion suggests that because mucoceles are pseudocysts there is no imperative to remove the cyst lining. Appropriate management should focus on identification and elimination of the salivary gland responsible for the source of mucus secretion (1). Removal of the stimulus for secretion should cause involution of the cystic cavity, which seals itself, naturally (7).
We would advocate that in cases of a submandibular gland mucocele the lesion should be excised via a cervical approach in conjunction with the submandibular gland. If any doubt exists as to the close involvement of the sublingual gland then it would be advisable to remove this gland as well.



