-
PDF
- Split View
-
Views
-
Cite
Cite
H Qandeel, H Abudeeb, A Hammad, C Murch, A Mukherjee, Colonic stent and percutaneous ethanol injection as a treatment for colocutaneous fistula secondary to benign stricture, Journal of Surgical Case Reports, Volume 2012, Issue 4, April 2012, Page 2, https://doi.org/10.1093/jscr/2012.4.2
Close - Share Icon Share
Abstract
We report successful treatment of colocutanteous stulae at the site of a benign colonic anastomotic stricture using Self-Expandable Metal Stents (SEMS) and Percutaneous Ethanol Injection (PEI). The stricture and the secondary stulae developed after Hartmann’s procedure for sigmoid diverticular abscess followed by reversal of the Hartmann’s procedure with a de-functioning loop ileostomy. Although there have been previously reported cases of SEMS for closure of malignant colonic stula, there are limited reports of SEMS for closure of benign colonic stulae and none of SEMS combined with PEI for benign colonic fistula. We conclude that this patient’s case exemplies the potential applications of SEMS combined with PEI as a feasible option of therapy for benign colorectal disease.
INTRODUCTION
Self-Expandable Metal Stents (SEMS) are uncommonly used for benign colonic disease because of their lack of removability and their high rate of migration. A retrievable stent may offer effective therapy for benign colorectal strictures (1).
CASE REPORT
A 54-year-old lady underwent emergency Hartmann’s procedure for diverticular sigmoid abscess. Histology had confirmed the presence of diverticular disease in the sigmoid colon along with inflammatory changes in the tubes, ovaries and part of the uterus, which was resected en-bloc. The patient subsequently underwent reversal of her Hartmann’s procedure with a de-functioning loop ileostomy.
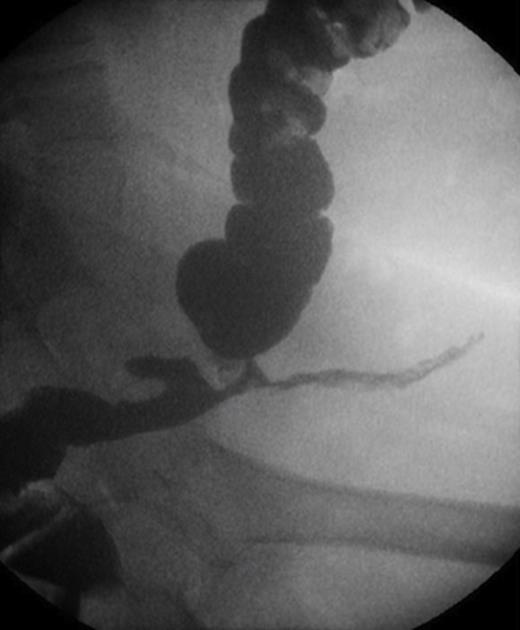
At a clinic review two months post Hartmann’s reversal, the patient complained of intermittent discharge from the lower end of her laparotomy wound associated with per-rectal intermittent discharge of mucous and blood. Contrast Studies had revealed the presence of an anastomotic stricture complicated with a colo-cutaneous fistula (Figure 1).
After a discussion with the patient, taking in account her obesity, the agreed plan was to adopt a non-operative approach rather than surgery that may result in a permanent end-colostomy. Three months post Hartmann’s reversal a balloon dilatation was carried out successfully via flexible sigmoidoscopy as a joint procedure with a specialist radiologist.
Four months post Hartmann’s reversal it was decided to repeat the dilatation then to insert a colonic stent along with Percutaneous Ethanol Injection (PEI) of the fistula. Covered SEMS was deployed successfully across the anastomotic stricture. This was followed by injection of 20mls of absolute Ethanol through the abdominal fistulous tract whilst, at the same time, normal saline was injected into the stent via a Foley’s Catheter to dilute the alcohol within the lumen of the colon. No complications were encountered.
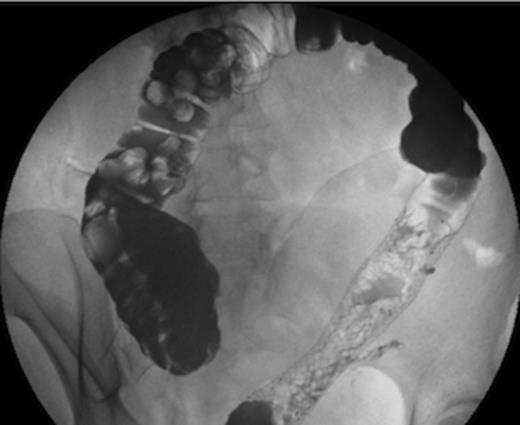
A month later, contrast studies showed complete resolution of the anastomotic stricture and no evidence of colo-cutaneous fistula (Figure 2). The SEMS was hence removed. At a clinic review one year post Hartmann’s reversal, the patient remained asymptomatic and the fistula had resolved both clinically and radiologically.
A year post Hartmann’s reversal, patient was admitted for reversal of her loop ileostomy, which was performed without complications. Follow up at 6 months later confirmed the absence of symptoms.
DISCUSSION
The use of self-expanding metallic stents for benign colorectal diseases has been regarded previously as controversial (1,2). This partly relates to a lack of published data. Only 3% of stents placed in 567 patients considered in a systematic review in (2002) were for benign disease, predominantly diverticular disease (3). There has been only a few reports of its use for closure of benign stulae in the colon (4).
In our case the presence of a stricture with stulous tracts was an indication for the use of a covered stent for immediate stula closure. Covered SEMS have a high rate of migration as compared to uncovered SEMS (2,5). In addition, spontaneous migration of SEMS for benign strictures occurs frequently, usually within the rst month after insertion (6).
Ethanol injection for successful ablation of digestive tract fistula has been mentioned in few case reports in the literature (7).
To our knowledge, this is the rst case demonstrating SEMS combined with PEI for benign postoperative stulae. Although longer follow up and future prospective studies are needed, this approach may offer an alternative therapy for patients unt for surgery.



